5 Client Encounter Framework
Kara Carmody
Framework for Client Encounter
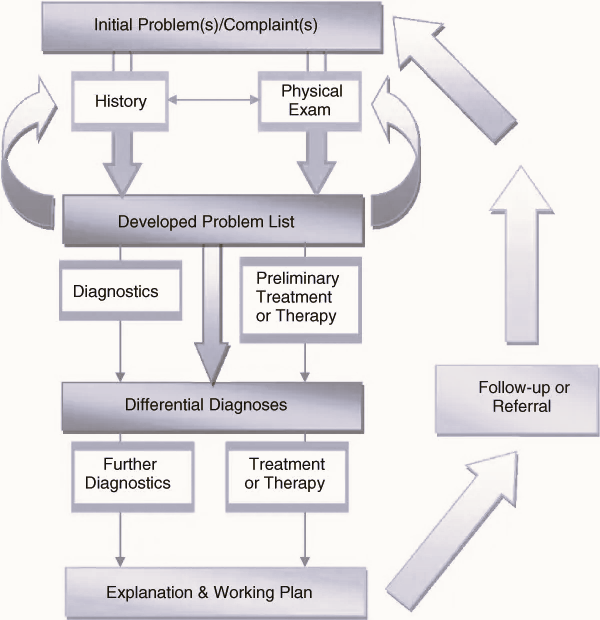
The framework discussed in this chapter is simply the expansion of the overarching structure we will refer and reference to as we move through the curriculum. Unfortunately, this graphic[1] is limited in its ability to convey the details and best practices for each of the individual components.
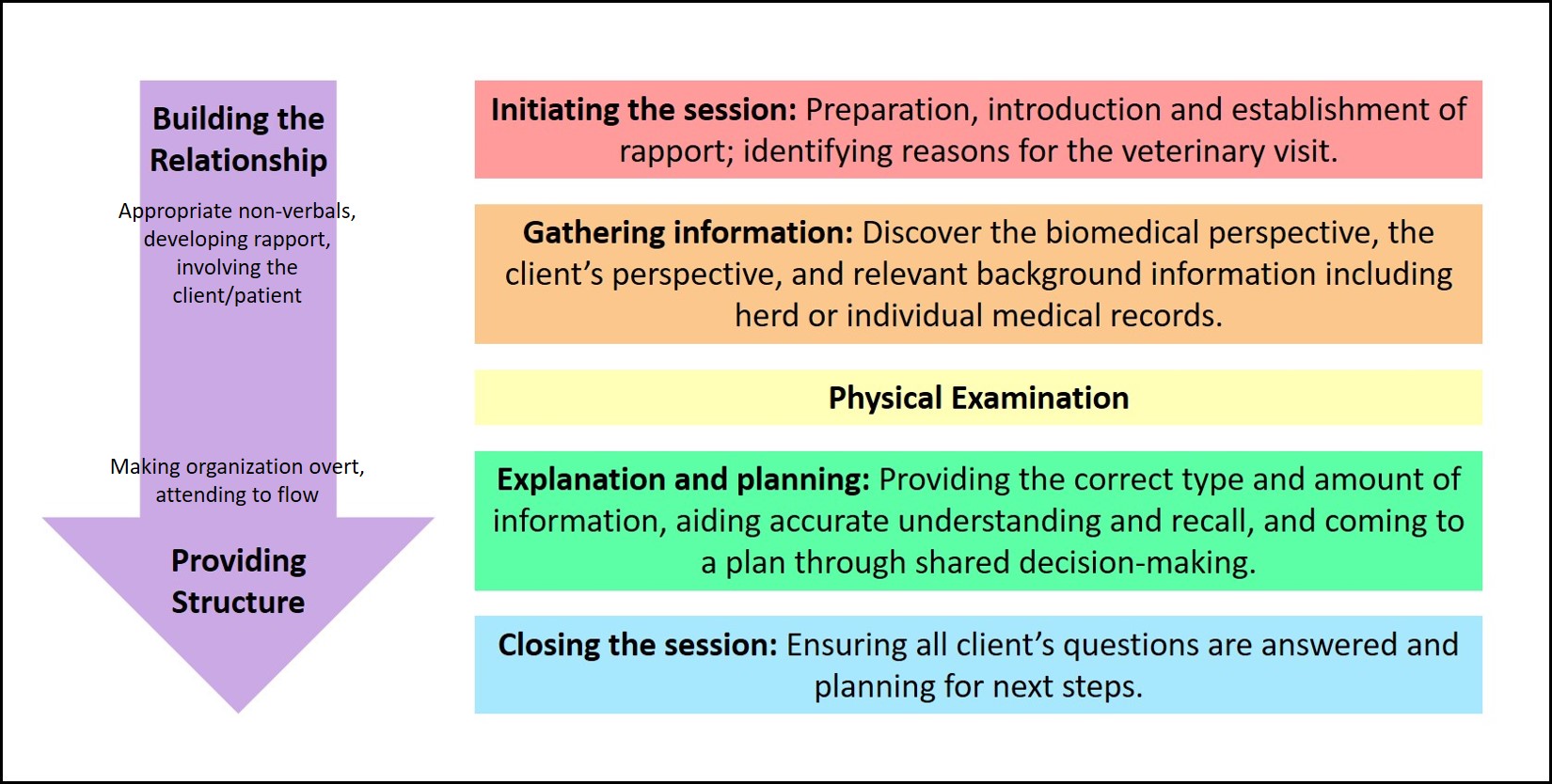
The following graphic provides another visual example of this pathway. A key take-away is to note, that while there is a linear and chronological theme to the encounter, there will be circumstances that require us to revisit individual steps of the pathway and that based on progression and outcomes, we may start again from the beginning.
Client and patient are greeted upon entering the facility and checked into the clinic system. Depending on the flow structure of the clinic/hospital, signposting can be used to direct the patient and client for seating/wait time/options available until their official appointment time begins.
When the patient care team (assistant, technician, veterinarian) are available, the official appointment encounter can begin. There are numerous models in practice regarding the roles of the assistants, technicians, and clinicians in the following framework. The following framework addresses the overall encounter and does not identify which member of the care team will fulfill this responsibility. This may vary from practice to practice as well as by appointment type or even based on staffing from day to day.
Initiating the Session & Gathering Information
- The client and patient are greeted with a formal introduction and ideally sign-posting for immediate next steps should occur (i.e., exam room, history taking, etc.).
- History gathering to include presenting complaints, general patient history, and most importantly client goals for the visit.
- Keys to success: implementing non-verbal communication techniques as well as open-ended questions, reflective statements, empathetic statements, and summarizing.
- Additional considerations for the care team include recognizing personal potential for bias as well as demonstrating cultural competence.
- Signpost to transition to the next step of the encounter
Physical Examination
Your ability to maximize the benefits of this diagnostic tool will be affected by numerous factors, primarily of which is patient temperament.
-
- Key considerations in this phase include minimizing patient fear, anxiety, and stress which often requires additional conversations with the client to troubleshoot problems or clarify information shared and building trust with the patient. Considerations to specific situations include:
- Evaluation of companion animals in a clinical setting (exam room/stall)
- Training the care team with Fear-Free Handling or a similar program creates a team that communicates and works with clients and patients in a consistent and effective format. https://fearfreepets.com/.
- Evaluation of a individual production animal (clinic vs on-site)
- The physical examination should always start with examining the animal from a distance. Observing gait, posture, and respiratory rate and effort when the animal is calm and not being restrained is necessary to obtaining the complete clinical picture. The ability to perform a physical exam will depend on the facilities available, the handleability of the animal, and the amount of help available to assist. The clinician must always consider safety for themselves, the patient, and others when working with large animals who may or may not be used to being restrained.
- Evaluation of a herd
- Assessing not just the individual animal(s) affected but also examining the rest of the herd can give the clinician more information sometimes than simply taking a history from the client. If the appointment is taking place on the farm, walking the property will give the clinician a sense for how the rest of the animals are doing but also allows for better assessment of housing, husbandry, and biosecurity practices of the farm.
- Evaluation of companion animals in a clinical setting (exam room/stall)
- Communication of exam findings may be done concurrently via narration or upon completion of the exam in summary or in some combination of both.
- Key considerations in this phase include minimizing patient fear, anxiety, and stress which often requires additional conversations with the client to troubleshoot problems or clarify information shared and building trust with the patient. Considerations to specific situations include:
Explanation and Planning
- Sharing the patient problem lists/differential diagnoses and/or hypotheses on underlying cause of the clinical presentation.
- Identify the most pressing problem(s) or a presumptive/working diagnosis as well as differential diagnoses.
- Hint: Sometimes the clinician may not **KNOW** a presumptive diagnosis.
- Identifying ‘what we know’ vs ‘what we don’t know’ can be a helpful strategy here.
- Essentially, the clinician is letting the client in on their train of thought.
- Acknowledge all problems presented by the client and communicate how they will be addressed.
- Keys to success: continued use of non-verbal communication techniques as well as chunk-n-check, ask-tell-ask, using simple language or defining medical terminology to be referenced as needed, visual aids.
- Information is conveyed with clarity and sensitivity.
- Identify the most pressing problem(s) or a presumptive/working diagnosis as well as differential diagnoses.
- Identify the tools (diagnostic tests) available to move the investigative process forward.
- The clinician will often consider a list of potential diagnoses (a differential diagnosis) when attempting to determine the cause of a patient’s presentation. The differential diagnosis represents a prioritized list of the top possibilities. Sometimes the most likely choice is designated to be the working diagnosis, meaning that it is likely, but hasn’t been confirmed, and that other diseases haven’t been ruled out. Typically, clinicians will consider more than one diagnostic hypothesis or possibility as an explanation of the patient’s symptoms and will refine this list as further information is obtained in the diagnostic process, eventually coming to a “working diagnosis.”
- The working diagnosis should be shared with the client, including an explanation of the degree of uncertainty associated with a working diagnosis. Each time there is a revision to the working diagnosis, this information should be communicated to the client, with opportunity for input and discussion.
- Be sure to acknowledge the benefits and/or limitations of the test as appropriate.
- Spectrum of Care approach is conveyed in the language used and presentation of options (i.e. avoiding “gold-standard” etc)
- Diagnostic testing may occur in successive rounds of information gathering, integration, and interpretation, as each round of information refines the working diagnosis.
- Describe plan of management or options, including diagnosis and treatment options/ alternatives to include supportive care therapy. This is an iterative process and will have varying levels of complexity based on the patient and problem(s). Successment plan implementation relies on collaboration with the client and the care team.
- Identify therapeutic plan (alternative to diagnostics or concurrent).
- Sometimes response to therapy is a diagnostic in its own right.
- Identify potential next steps.
- If/then scenarios, keep these at a ‘high altitude’.
- Keys to success: continued use of non-verbal communication techniques and summarizing
- Information is conveyed with confidence and clarity.
- Identify therapeutic plan (alternative to diagnostics or concurrent).
- Assess the client’s understanding and negotiate an agreed upon plan of action.
- Risks of procedures should be discussed and informed consent to include procedures and financial estimates should be obtained and documented.
- Keys to success: use of simple language, chunk-and-check, summarizing, open-ended questions to invite client-initiated questions.
**Usually, some amount of time will pass, hours or even days depending on the test turnaround time. ***
- Present Diagnostic Results
- Communicate the test results and the implications of those results as well as any ambiguity of results.
- Keys to success: continued use of non-verbal communication techniques as well as chunk-n-check, ask-tell-ask, using simple language or defining medical terminology to be referenced as needed, visual aids
- Deliver Diagnosis
- A required element of the diagnostic process is to communicate to the client an explanation of the patient’s health problem. Sometimes this will be a single diagnosis. Other times it may be a class or category within a broader health issue, such as ‘an upper respiratory tract infection’. Or, as discussed above, several different diagnostic possibilities may remain, and these may be narrowed down over time by further testing, or consultation, or by waiting to see if the clinical signs worsen or improve, or if new ones arise.
- Keys to success: continued use of non-verbal communication techniques as well as chunk-n-check, ask-tell-ask, using simple language or defining medical terminology to be referenced as needed, visual aids
- Discuss Treatment Options
- This is the planned path of care based on the diagnosis. Sometimes this may be a treatment trial if the diagnosis isn’t certain, and other times it may be appropriate to defer specific treatment until the diagnosis is more certain. In addition, supportive care treatments that have not already been discussed/started would be appropriate to mention here.
- Keys to success: continued use of non-verbal communication techniques as well as chunk-n-check, ask-tell-ask, using simple language or defining medical terminology to be referenced as needed.
- Client Education
- Depending on the diagnosis, treatment plans elected, etc., this conversation may vary significantly in complexity.
- The keys to success in communication remain the same in an effort to provide the client with helpful information in the most efficient manner.
- Additional written resources in the form of client handouts, personalized discharges, or outside websites are crucial in order for clients to have opportunities to reconnect with the information, in a format consistent with what you shared. If these resources are not available, they will often seek them independently and misinformation on topics is often widespread.
- Identify follow-up plan
- Expectations for both the client and the care team (test turnaround time, results call backs, call backs to check-in, recheck visits, if/when clinical signs to monitor and next best steps scenarios should be reviewed, challenges with ability to implement treatment plan, etc.).
- Discuss costs
- This ideally can be integrated into the points above but can also be discussed at a separate time with a written estimate if that is more conducive to the encounter flow in your specific practice.
Closing the Session
- Confirm agreement/approval from the client
- Open-ended questions can be used, however close-ended questions are also appropriate to clearly confirm approval.
- Sign-post immediate next steps.
- Close the episode to the client’s satisfaction usually through an open-ended question to identify any outstanding client concerns such as “What other questions/concerns do you have for me?”.
Medical Record
The client/patient encounter should be documented in a written SOAP note which facilitates communication for all members of the veterinary care team. All of the communication that takes place with the client must be documented in the medical record. See Medical Record Keeping for more detailed information.
Evaluate Outcome/Clinician Reflection
One of the most powerful learning tools we have for professional growth is self-reflection. Taking the time to reflect on client encounters (both those that went well and those that could have been improved) will only position you to become a better communicator and clinician over time. Keys to consider include:
- Client satisfaction: Despite even a negative health outcome, if the client is satisfied with the outcome, then you have been successful in your role as clinician
- The outcomes of the diagnostic process are also extremely important. Considering veterinary patients we have an additional layer (client observations, expectations, adherence) to navigate to effectively treat/manage patients. In reflection, were your communication skills such that it improved the likelihood of identifying the health problem correctly, resolving the clinical signs, achieving an appropriate health outcome for the patient (i.e. treatment vs euthanasia vs other).