9 Regulatory Basics
William Durfee and Paul Iaizzo
Defining ‘Medical Device’
Before looking regulations, ‘medical device’ must be defined. Medical devices are exceptionally broad, and include everything from a bandage to a robot surgery system.
In the USA, regulation of medical devices is done by the Center for Devices and Radiological Health (CDRH), a division of the Food and Drug Administration (FDA). Use the FDA site (http://www.fda.gov/MedicalDevices) to help you get started on medical devices and their regulation.
The FDA definition of a medical device:
“An instrument, apparatus, implement, machine, contrivance, implant, in vitro reagent, or other similar or related article, including a component part, or accessory which is:
recognized in the official National Formulary, or the United States Pharmacopoeia, or any supplement to them,
intended for use in the diagnosis of disease or other conditions, or in the cure, mitigation, treatment, or prevention of disease, in man or other animals, or
intended to affect the structure or any function of the body of man or other animals, and which does not achieve any of its primary intended purposes through chemical action within or on the body of man or other animals and which is not dependent upon being metabolized for the achievement of any of its primary intended purposes.”
Medical Device Class
The FDA divides medical devices into three categories depending on risk:
- Class I: Low Risk
- Bandages and crutches.
- Class II: Intermediate Risk
- Power wheelchairs, guidewires and stents.
- Class III: High Risk
- Drug delivery pumps, heart valves and deep brain stimulators. Typically life sustaining devices.
Determine the Class of Your Device
One part of the FDA site (http://goo.gl/ryjJk) guides you in how to determine if your device is Class I, II, III. Follow the links and find the name of your device. The description of the device will include the classification.
For example, from the Device Classification Panels page (http://goo.gl/L8l1G), Part 870 Cardiovascular → Subpart D – Cardiovascular Prosthetic Devices → 870.3925 – Replacement heart valve, takes you to the page (http://goo.gl/eO68y), where you can find out that a replacement heart valve is a Class III device that requires premarket approval.
Regulatory Approval
Class I Devices
Most Class I (low risk) devices fall in the FDA’s exempt category, which means FDA clearance is not required for marketing. For example, new tongue depressor does not require FDA approval. However, even if exempt, Class I devices must still be registered with the FDA and must follow the “general controls” established by the FDA, which among other things establish manufacturing standards and labeling requirements that must be followed.
Class II Devices
Many Class II (moderate risk) devices can use the 510(k) pathway for approval. Here the manufacturer must demonstrate that the new device is “substantially equivalent” to a predicate device that is already on the market. The concept is that if there is a device already being sold that has FDA approval, there is no need for the new device to independently prove that it is safe and effective.
To receive approval (called a “clearance”) under 510(k) the new device is compared to the predicate device using the following questions:
- Has the predicate device been cleared under the 510(k) process?
- Do the new device and the predicate device have the same intended use?
- Do the two devices have similar technical characteristics?
- If the technical characteristics are different, do the new features raise questions of safety and effectiveness and has data been provided that the new device is at least as safe and effective as the predicate device?
In making its substantially equivalent case, the applicant typically relies on data from bench testing and animal testing. Some devices can prove equivalence just from careful bench tests. Human testing is rarely needed and when requested by the FDA generally involve clinical studies with a small number of patients.
If the FDA agrees with the applicant that the new device is equivalent to the predicate, it will issue a Substantially Equivalent (SE) letter. If not it will issue a Not Substantially Equivalent (NSE) letter and the device will then be automatically placed in Class III.
Class III Devices
Class III devices go through the pre-market approval (PMA) process, which requires demonstrating that the new device is safe and effective in humans. A PMA requires substantial and costly clinical trials in human subjects.
Investigational Device Exemption
In order to enable research studies using human testing before the device is approved through the 510(k) or PMA process, investigators apply for an investigational device exemption (IDE). A non-significant risk device can be approved for research use by the local institutional review board (IRB). A significant risk device must be approved by the IRB and by the FDA.
In Europe
To obtain CE mark prior to marketing a device in Europe, the regulatory process is primarily about safety, letting the market determine whether the device is effective.
Regulatory Process is Significant
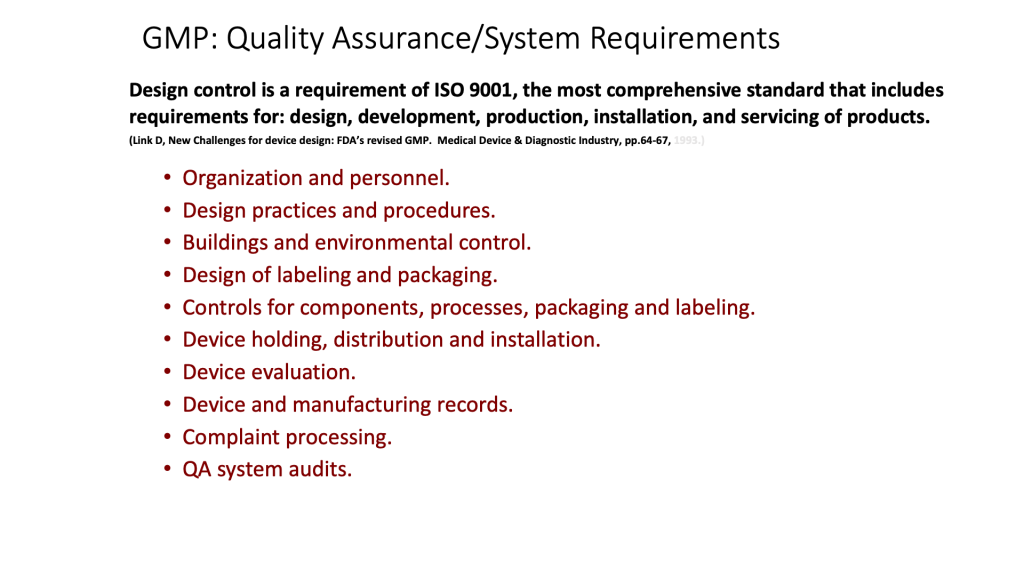
For the regulatory process one should also consider the FDA guidelines on “Good Manufacturing Process (GMP)”.
Some of the controls one needs to consider with GMP:
Importantly, the regulatory processes, guidelines and requirements will differ from country to country and be continuously updated by the various regulatory bodies around the world. Despite this, in general, the various international regulatory boards require:
- Evidence to support the claims
- Evidence that the technology is safe and effective
- Scientific evidence to back up the claim that a technology is cost-effective
“Cost-effective” does not necessarily mean inexpensive. An expensive technology that saves in overall healthcare costs because of improved outcomes can be considered cost-effective.
Here is what the innovator needs to do about regulatory issues:
- Be well informed
- Start early
- Initiate communication with the appropriate regulatory body, e.g. the FDA
- Use internal and external advisors
- Be global

