5 Parasite Control
Learning Objectives
- Describe fecal flotation testing, including fecal egg counts and fecal egg count reduction testing
- List common internal and external parasites of concern in common domestic species
- Describe life cycle of representative parasites as it pertains to control
- Describe drugs and mechanisms used for parasite control in common domestic species
- Define refugia
- Describe pasture management for parasite control
*
Parasite Infection and Tools for Diagnosis
Parasites, either internal (for example, worms) or external (for example, fleas and ticks), draw nutrients away from the host, and can cause disease. This chapter will focus on demonstration of how your understanding of the life cycle of parasites for various species in different environments will help minimize infection or infestation and help with control of the parasite in the environment. The biggest difference appears to be in overall management between large animals and small animals. In large animals, there is concern about resistance of parasites to available deworming medications and great attention is paid to minimizing development of resistant parasites. This may include leaving a small population of worms untreated, so there always are susceptible worms in the overall population and we are not just continually killing off susceptible worms and leaving behind more and more resistant worms. In small animals, where parasites can be a significant public health concern, it is a goal to kill all internal and external parasites. This does not mean there are no concerns about resistance; in 2021, resistance in hookworms, one intestinal parasite of dogs, was described.
Gastrointestinal parasites are the class most commonly addressed. Some common tools used to evaluate presence of gastrointestinal parasites are fecal flotation tests and fecal egg counts. Fecal egg counts are basically quantified fecal flotations. You will also hear fecal flotations called fecal floats. Dr. Erin Burton provides the following differentiation between these two kinds of tests and how they’re interpreted: A fecal flotation is a qualitative assessment of the eggs in a sample, while a fecal egg count (FEC) is a quantitative assessment. Fecal flotations are lax on the amount of solution and feces used for each float and so give at best a semi-quantitative assessment of egg burden. FECs use a measured amount of feces and solution, and then plug the number into a formula to get the egg count. FEC usually is done more than once; in order to interpret them they are performed over time and because of that they are the test primarily used to definitively define the degree of drug resistance in an animal or herd. It is also important when evaluating a fecal float or FEC to be aware of how prolific of an egg layer the nematode is. For example, one Toxocara canis (roundworm) can produce over 20,000 eggs each day while a whipworm only produces about 1000 per day. Thus, having larger numbers of whipworm eggs on a float or FEC is more indicative of a heavy worm burden than abundant Toxocara eggs on float or FEC. Finally, be aware that not all gastrointestinal parasites can be identified by fecal flotation testing. For example, tapeworm eggs generally are released within tapeworm segments, or proglottids, and because the individual eggs are not in the feces and the proglottids are too heavy to float, tapeworm infections generally cannot be diagnosed by fecal flotation testing.
*
 Beef Cattle
Beef Cattle
Parasites can have potential negative effects on beef cattle that can vary from subclinical immune suppression, irritation, annoyance, appetite suppression, and decreased production, to severe clinical disease and death. The management of parasites is a component of a preventive health program that should also include immunity management (vaccinations), management procedures, handling, and nutritional considerations that reflect an in-depth understanding of not only the beef production system but farm-specific issues and goals.
Internal Parasites
Internal parasites include roundworms (nematodes), tapeworms (cestodes), flukes (trematodes) and protozoans (such as coccidia). Roundworms are considered the most economically important, and many programs revolve around their management. This section regarding internal parasites in beef cattle will focus around roundworms. Understanding the parasite life cycle and the level of parasite pressure is key to the management of internal parasites.
The following is the basic life cycle of internal (gastrointestinal) parasites in cattle:
- Adult parasites live in the gastrointestinal tract of cattle and lay eggs that are shed in the manure.
- When a parasite egg is shed on the pasture in the feces, this egg begins development, embryonating into a first stage larva (L1), then molting into a second stage larva (L2), and finally molting again into a third and infective stage larva (L3).
- During the first two larval stages in the fecal pat, the larva are fairly immobile, feeding off the bacteria and other debris found in the feces.
- During the third larval stage the larva move out of the fecal pat and onto nearby grass where they are consumed by cattle.
- L3 larvae maintain an external sheath covering that provides extra protection from environmental conditions allowing survival during winter or drought conditions. This sheath prevents feeding, thus L3 larvae have a limited life span.
- Egg development is greatly dependent upon temperature and moisture. Eggs that are passed in the middle of winter will not develop until warm weather returns in the spring. Eggs passed in the middle of a drought or other unfavorable conditions may develop into infective larvae in the feces but without moisture cannot move away from the pat where they can be consumed by a host animal when it eats grass. Eggs that are shed during favorable conditions can develop into infective larvae in just a few days if temperatures are warm and moisture is plentiful.
- Once consumed by cattle, the infective larvae mature into adults over a period of 3-4 weeks (shorter in younger cattle, longer in adult cattle) and begin to lay eggs, which are shed onto pastures to start the cycle over again.
- Some larvae can become inhibited or hypobiotic (go into hibernation) in the wall of the abomasum, sometimes referred to as L4 larvae. This process can occur during the winter in the north and in the summer in the south, with these larvae maturing and developing into adult worms when the environment for egg survival is more favorable.
Overall, the controlling of internal parasites has a significant positive return on investment for producers. The main focus of internal parasite control in beef cattle is roundworms. Diagnostics are needed to determine which specific worms are present. For beef cattle this is important because the roundworm life cycle depends on the shedding of the eggs on pasture, larvae development, and the ingestion of the larvae during grazing. Since much of beef cattle production depends on grazing of pastures, the management of roundworms is key. As long as cattle have access to grass, they will have an internal parasite challenge.
Control practices should consider the class (or age) of cattle, nutrition status, stress level, season, and likelihood of parasite contamination of the environment, and involve the use of pasture management options as well as the use of anthelmintic (dewormer) products for treatment.
Life-Cycle of Internal Parasites
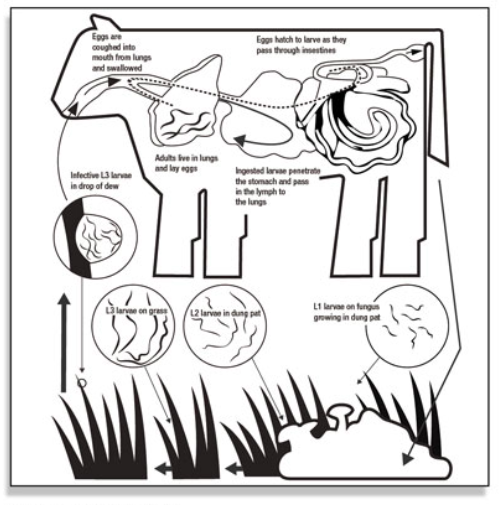
- Infective L3 larvae in a drop of dew enter the cow’s mouth when eating grass.
- Ingested larvae penetrate the stomach and pass in the lymph to the lungs.
- Adults live in lungs and lay eggs.
- Eggs are coughed into mouth from lungs and swallowed.
- Eggs hatch to larvae as they pass through intestines.
- L1 larvae on fungus grow in dung pat.
- L2 larvae live in dung pat.
- L3 larvae move onto grass where they again can be ingested by cows.
Parasite Contamination Susceptibility
| PRIORITIZED SUSCEPTIBILITY TO PARASITES | ENVIRONMENTAL PARASITE CONTAMINATION LIKELIHOOD |
| Calves > Yearlings > Adult bulls > Adult cows | Spring / Early summer > Late summer (dry season) > Winter |
| Nutritionally challenged > Not nutritionally challenged | Continuously grazed pasture > Rested pasture > Not grazed / Hayed pasture > Recently tilled > Dry lot |
| Stressed (newly weaned, heat/cold stress, etc) > Not stressed |
Some pasture management activities may include leaving the pasture fallow, grazing other species, and dragging manure pats during the dry season to allow them to dry out.
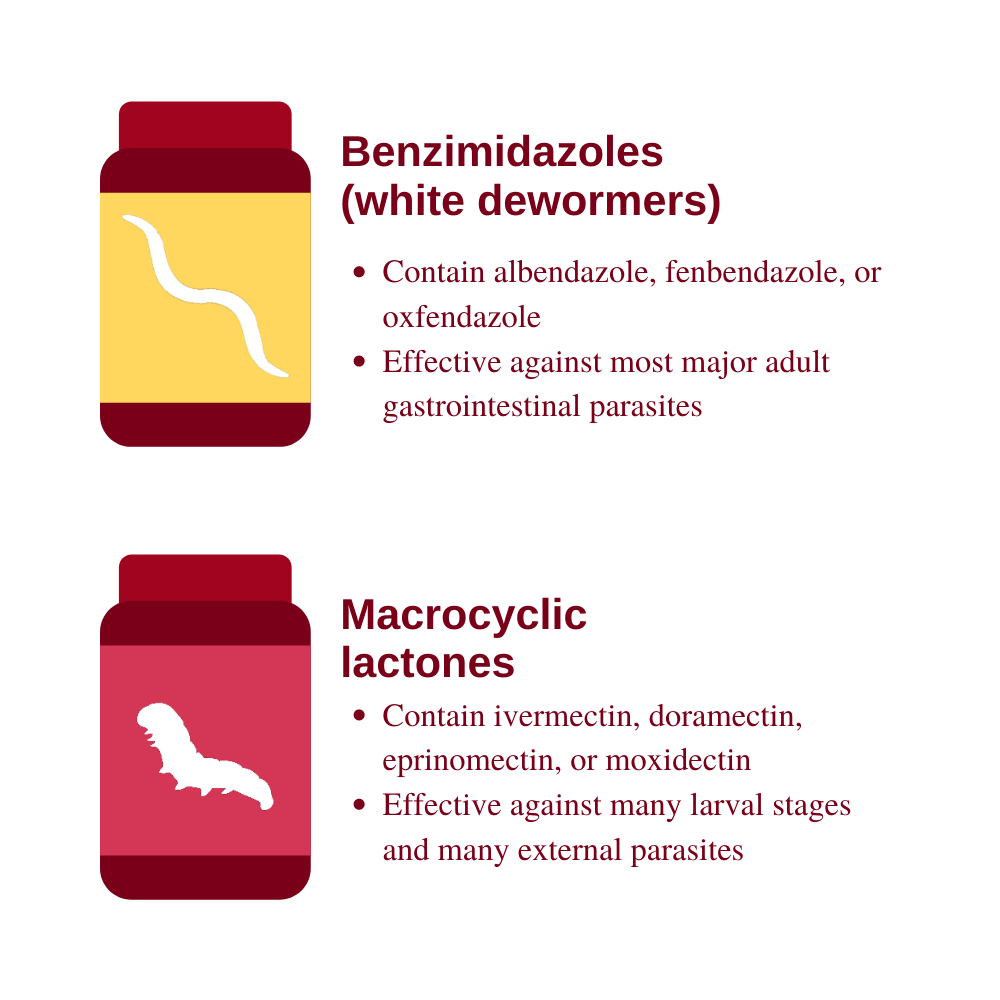
Anthelmintics used to control internal parasites for beef cattle come in several forms including paste, injectable, drench, pour-on, bolus, and as a feed or mineral additive. Products have varying lengths of activity and costs, but fall into two main classes: benzimidazoles and macrocylic lactones. Benzimidazoles (white dewormers) available commercially contain albendazole, fenbendazole, or oxfendazole. Benzimidazoles are effective against most of the major adult gastrointestinal parasites and many of the larval stages. Products come in various oral formulations and have a short duration of efficacy. Macrocyclic lactones are the avermectins and milbemycins. Products in commercial use contain ivermectin, doramectin, eprinomectin, or moxidectin. The macrocyclic lactones have a potent, broad antiparasitic spectrum at low dose levels. They are active against many larval stages (including hypobiotic larvae) and are active against many external parasites as well. Products are available as oral, subcutaneous, and pour-on formulations for use in cattle. Duration of efficacy varies with the product and may be up to 35 days.
Approaches used to treat parasites in beef cattle are considered strategic deworming. This is the practice of treating cattle at times to not only get the benefit in that animal to prevent economic loss but also reduce environmental contamination for a period of time at least equal to the life cycle of the parasite removed.
Keys to strategic deworming are to place cattle that are not shedding eggs on pastures that are not infected; this is accomplished by deworming prior to spring turnout or fall treatment in the north (following killing frost). The benefit of treating in the fall is that cattle should be free of internal parasites all winter and going into the spring turnout (assuming an effective product was used). Cattle that go onto pasture at spring turnout are free of parasites, thus not shedding eggs, and will be consuming the infective larvae on the pasture if the pasture is contaminated. By consuming the infective larvae and not shedding new ones the cows will be reducing the load on the pasture (acting as vacuum cleaners). After a time the ingested infective larvae will mature and cows will start shedding eggs. Strategic deworming times the treatment so as to reduce the worm burden on the cattle and also decrease the parasite contamination of the pasture during the highest parasite period (spring/early summer).
The timing of these treatments can and should be timed with other management procedures such as summer vaccines for the calves and fall processing of calves and cows. Depending on the geographic location, such as in the south where the weather (moisture) is different, timings may be different, as well as the type of grazing program.
Calves and stockers should be considered within a strategic program while on a grazing program. Times of concern include prior to weaning while nursing the cow and while intensively grazing as a stocker. Calves should not be dewormed while being weaned. Preweaning treatment, prior to the stress of weaning, can reduce the potential negative impact on immune function as well as improve performance. Any time cattle are moving from pasture into a dry lot setting is a good time to deworm as this should clear cattle of parasite load for the time in the dry lot (similar to fall deworming) as there is no green grass to graze.
For the control of other types of internal parasites such as tapeworms (cestodes), flukes (trematodes), and protozoans (such as coccidia), similar concepts are applied. It is important to understand the different life cycles of these different types of parasites as well as the efficacy of products used to treat them.
External Parasites
The major external parasites that affect cattle include flies, grubs, lice, ticks, and mites. These external parasites feed on body tissues such as blood and skin, and in addition they cause irritation and discomfort that result in reduced weight gain and lost production. Parasites that take blood meals have the potential to serve as vectors for the transmission of diseases.
Horn Flies
Horn flies are blood-sucking flies that stay on the shoulders and backs of cattle almost continuously. A horn fly leaves the back of a cow or calf only to lay eggs in fresh manure. They take blood meals from the host 24 hours a day.
Face Flies
Face flies cluster on the faces of cattle and feed on secretions from the mucous membranes of the eyes, nose, and lips. Face flies do not suck blood. They do irritate the surface of the eyeball and may carry pathogens that contribute to pinkeye problems. They spend only a small portion of their life on cattle.
Stable Flies
Stable flies feed primarily on the legs and lower abdomen of cattle and take blood meals two to three times a day depending on the weather. After feeding they move to a resting place to digest the blood meal. Stable flies are associated with substantial economic loss in cattle from the blood loss and pain from feeding. As few as five flies per leg is economically significant in cattle.
Ticks
Ticks cause blood loss and discomfort, and can act as vectors for disease spread. High concentrations of ticks usually occur in brushy pastures and woodlands.
Lice
Lice that affect cattle are either of the biting or sucking type, and cause skin irritation and itching. The entire life cycle of lice is on the host and they are present year round but populations increase in winter months. Lice spread through contact with infested cattle. Infested cattle can experience reduced appetite and anemia, and appear unthrifty.
Mites
In cattle, mites can cause hair loss and a thickening of the skin. Infestation by mites is called mange. Mites are spread by close contact. Severe mange can weaken cattle and make them vulnerable to diseases. Certain types of mites are reportable.
Cattle Grubs (warbles)
Cattle grubs, or warbles, are the larval stage of the heel fly. The larvae migrate from the animal’s heel, where the eggs are deposited by the adult fly in early summer, to the back of the animal. The larvae can cause damage to the hide (due to the breathing hole they create) and if treated during the wrong time of the year can cause paralysis due to their location near the spinal column. Cattle should not be treated with a grubicide between November 15 and March 1 if cattle grubs are a concern.
Control of External Parasites
Control of external parasites usually revolves around the use of insecticides. These usually are a pyrethrin or an organophosphate. Strategies or combinations of strategies for delivery include: dust bags, back-rubbers (oilers), animal sprays, pour-ons, and insecticide impregnated ear tags. In addition, the use of injectable products or pour-ons with systemic activity work well to control lice and mites. Larvicides can also be part of control plan for certain types of flies as well as the use of predator wasps and environmental management. The use of dust bags and back-rubbers (oilers) can provide delivery of insecticides and economic fly control if located in an area that cattle are forced to move through such as a gateway or over a mineral feeder.
Delivery of Insecticides
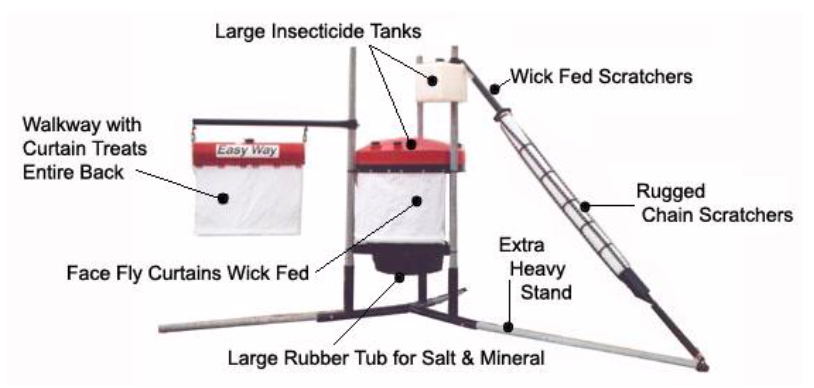
Insecticide sprays and pour-ons are effective for many different external parasites but have the drawback of increased animal handling costs and stress during the fly-season. Insecticide sprays are the only way to manage adult stable flies. Ear tags impregnated with insecticide can be effective in fly control. Maximizing control requires two tags per animal, and timing of application with peak fly numbers often requires a separate handling session of the animals. Ear tags provide good face fly control if applied properly.
Insecticide Ear Tag Fly Control

Larvicides prevent fly larvae from developing in to adults and are administered through free choice mineral. To be effective cattle must consume an adequate amount and not be in the proximity of untreated cattle.
Injectable products and pour-ons with systemic activity are mainly the macrocyclic lactones. These are effective against some flies as well as mites and lice. For mites and lice a second treatment may be needed in two to three weeks to kill newly hatched parasites unless using an extended duration product.
Sanitation or cleaning up of wasted feed or manure that serve as egg-laying sites for certain flies can greatly contribute to the control of certain flies locally. In addition, egg laying sites may be treated with a larvicide.
Environmental management may be a key component to tick control. The reduction of brushy areas and thick wooded areas reduces the habitat for the ticks and reduces exposure.
Certain native parasitic wasps are used as biological control agents of fly populations. Currently, farmers can buy parasitic wasps from commercial insectaries. These wasps emerge into adulthood from the pupal stage, where they develop wings. They fly from the release stations in which they have been held, hung from barn ceilings or other out-of-reach places. The wasps only target flies in their pupal stage. When the wasp finds a pupa in soil or litter, she inserts her stinger and withdraws it, drawing blood and paralyzing the pupa and inserting one egg. The egg hatches after 1 day, and the larva feeds on body fluids and organs for 2-4 weeks. Eventually, the wasp chews its way out of the dead host’s puparium and flies away as an adult.
Example Strategic Control Program
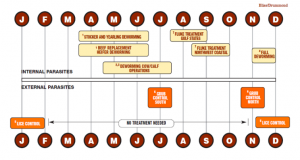
- Stocker, yearling and replacement heifers dewormed at turnout, four and eight weeks after onset of grazing (0-4-8).
- Cow/calf deworming six weeks after onset of grazing.
- If cattle were not dewormed in the fall, adult cows should be dewormed at pasture turnout and again six weeks after onset of grazing.
- All cattle retained over winter should be dewormed.
- During lice season, two treatments two to three weeks apart may be necessary.
- Grub treatment three to four months after the end of heel fly season, varies south to north. Requires systemic, annual control only.
- Cattle grazed along the Gulf Coast and Northwest coast should be treated for adult and immature liver flukes.
(Horn-fly control as needed to keep populations below 200 flies per animal.)
There is increasing evidence of antiparasitic resistance in grazing species, such as cattle, small ruminants (sheep and goats), and horses, both globally and within the United States. Antiparasitic resistance is the genetic ability of parasites to survive treatment with an antiparasitic drug that was generally effective against those parasites in the past.
Many factors contribute to antiparasitic resistance, including the biology of the parasite; the immune status of the host animal; treatment practices; drug properties; and certain livestock management practices. To help combat this emerging problem, the FDA’s Center for Veterinary Medicine started the Antiparasitic Resistance Management Strategy (ARMS).
*
 Dairy Cattle
Dairy Cattle
As in beef cattle, the overarching theme for the prevention strategy of parasitic infection is to reduce the animals’ exposure to parasites and their infectious forms. Because multiple animals will be exposed, any strategy will focus on entire groups of animals rather than individuals. So far, this is similar to prevention strategies for any other infectious diseases on farm. However, when thinking about the prevention of parasite infections on farm, the veterinarian must be aware of the infectious form of the parasite (for example, eggs versus larvae) and whether or not other hosts are involved in the life cycle. Then the best parasiticide is selected and management practices, such as grazing schedule, are properly timed to avoid exposure to infectious parasite forms in the environment. In most cases, prevention strategies therefore boil down to good on-farm hygiene and use of well-timed and correctly selected dewormers, as well as pasture management as described for beef cattle. There are different forms of deworming medications for dairy cattle. For simplicity of application, many are pour-ons or feed additives; some are injectables. Oral pastes or any formulation that requires you to handle the animals’ heads is rarely used because it is labor-intensive. Any product used in an animal that may be used for milk or meat has a specific withdrawal time. Withdrawal time is defined as the period from when the drug was used until the milk may be put in the bulk tank or the animal sent to slaughter for meat. How long the withdrawal time is and whether you can use a given drug in a lactating cow depends on the product. One thing that people might not be aware of – once a cow has calved for the first time, she is always considered to be a lactating animal, even if she’s not being milked (dry period). Always, always, read the label to know what the product will treat for, at what dosage and frequency it should be used, by what route it should be administered, what class of animals it is for, and withdrawal times.

*
 Small Ruminants
Small Ruminants
In general, the number of internal parasites in sheep and goats will increase with number of host animals (higher stocking rate); during warm, humid weather; and when pastures are grazed too short. The number of internal parasites will decrease in hot, dry weather; if a non-host animal (cattle or horses) grazes the same pasture; or if the pasture has been rested (no grazing, larvae die off naturally).
Some worms in a population will survive even the most appropriate drug treatments. This is due to genetic selection for resistant worms in a treated population. Modern dewormers are effective, broad in spectrum, cheap, and safe but people have relied more on drugs than on husbandry as a way to control parasites, leading to increased parasite resistance. To minimize development of parasite resistance to dewormers, use treatments specifically and selectively.
Clinical signs of parasitism in sheep and goats include diarrhea, bottle jaw (submandibular edema secondary to hypoproteinemia), anemia, and rough hair coat. Subclinical effects of parasitism include reduced weaning weight, reduced milk production, reduced reproductive performance, reduced growth rate, and increased susceptibility to disease.

Treatment of sheep often includes drenching. The veterinarian should perform diagnostics to determine type of parasite(s) present. You may wish to perform a fecal egg count before and after treatment (fecal egg count reduction test) to determine how effective your treatment was. Weigh the sheep and prepare the dewormer based on weight. Deliver the dewormer over the tongue in the back of the throat with a drench tip or drench gun.
To determine who needs to be dewormed, veterinarians can do a fecal egg count (FEC) to measure number of worm eggs per gram of feces (epg). General class of parasites is identified (for example, strongyle-type) but the specific parasite rarely is identified (it is difficult to differentiate between Haemonchus, Teladorsagia (formerly Ostertagia), and Trichostrongyles). One recommendation for goats is to deworm bucks and dry (non-lactating) does if there are more than 2000 epg, lactating does if there are more than 750 epg, and all other animals if there are more than 1000 epg. Not all of the animals in the herd will be carrying parasites to the same extent and schemes exist that permit veterinarians to assess the animal clinically and from that, determine which individuals in the herd should be dewormed. This prevents treating animals unnecessarily, which is better for their health and less expensive for the owner, and helps prevent development of resistant parasites by minimizing use of deworming medications.
Not treating all animals also means you’re leaving a certain number of untreated worms in the population; because these worms have not been exposed to dewormer, you’re allowing them to persist and maintaining a more genetically diverse worm population. This population of untreated worms (called refugia) can be a valuable thing to consider when facing problems with anthelmintic resistance.
FAMACHA© is a diagnostic test to help small ruminant producers identify animals that require anthelmintic treatment and those that do not require deworming. The tool is a card that matches eyelid color to anemia levels, an indicator of clinical infection with parasites that cause anemia. A good resource about FAMACHA testing and general information about parasite control in small ruminants is the American Consortium for Small Ruminant Parasite Control.
As in cattle, pasture management is another important component of parasite control. To stop the parasite life cycle, remove sheep and goats from pastures for 3-6 months to allow worm larvae in the pasture to die off. Alternate or co-graze pastures with horses or adult cattle. Maintain stocking rates of no more than 6-8 sheep or goats per acre.
General considerations for parasite control include:
- Do not overgraze pastures; the vast majority of infective nematode larvae are on the first 2” of vegetation for a given plant.
- Spread manure in hot, dry conditions to kill worm eggs and larvae that may be in the feces.
- Rotate crops and livestock.
- Ensure a high plane of nutrition for ewes/does and lambs/kids.
- Use body condition score and other clinical signs to monitor flock health.
*
 Swine
Swine
Management and housing techniques used in modern commercial pig production, as well as the prudent use of anti-parasitic products, has dramatically reduced, and in many cases, eliminated the disease and animal welfare issues associated with parasite infections in pigs. Although parasites are no longer a significant challenge to the majority of pigs being produced in North America, they continue to play a role in some types of pig production, primarily in those animals exposed to outdoor environments. Therefore, a solid understanding of their types and prevention are important.
Internal Parasites
Categories of internal parasites include nematodes (roundworms), thorny-headed worms, tapeworms, and protozoa. Ascarus suum (a nematode or roundworm) and coccidia (a protozoan) are the most common internal parasites in commercial pig production at this time.
External Parasites
Categories of external parasites include ticks, mites, lice, mosquitoes, and flies. Mosquitoes and flies continue to be common challenges in both indoor and outdoor pig production while ticks, mites, and lice are primarily limited to pigs that are raised outdoors. Mosquitoes and biting flies are known to mechanically spread important diseases between groups and premises.
Prevention of Parasite Infections
Key factors to consider for the prevention of both internal and external parasite infections include:
- Source negative pigs
- Knowledge of negative parasite status of replacement breeding stock prior to purchase and the prevention of moving positive stock into negative herds
- Minimize dose or eliminate exposure completely
- Indoor production eliminates access to normal source of infection
- All in-all out production: regular emptying of facilities between production groups
- Sanitation: regular cleaning of facilities using appropriate detergent and disinfectant between production groups
- Eliminate areas where external parasites can breed and develop (e.g. elimination of standing water reservoirs decreases mosquito levels)
- Monitoring program to insure early identification
- A good monitoring program allows the early detection of a parasite challenge and the early application of intervention strategies.
- This may include a routine fecal sampling program, observation of clinical signs, and gross signs on routine post mortems or slaughter checks.
- Therapeutic prevention programs
- Strategic preventive therapy programs are commonly used to treat parasite infections so that the challenge to the individual and challenge to herd mates (via shedding) is minimized.
*
 Horses
Horses
The internal parasites of greatest importance among North American horses are small strongyles (cyathostomes), large strongyles, ascarids (roundworms), tapeworms, and bots. Strongyles and ascarids are transmitted via a direct fecal-oral route, tapeworms have a more indirect fecal-oral transmission pattern involving the orbatid mite as intermediate host, and bots are transmitted when horses ingest fly eggs deposited on the hairs of their front legs. Small strongyles, ascarids (in young horses under 2 years of age), and tapeworms are the main focus of an equine parasite control program, as they have the greatest potential to cause disease. Bots rarely cause disease and are generally well controlled as a side benefit of the control program used to control strongyles and ascarids.
Ascarids (Parascaris equorum) are a significant health risk for foals, weanlings, and yearlings, but not for adult horses due to development of age-related immunity. Adult horses within a given herd can vary greatly in their susceptibility to parasite infestation, especially with respect to small strongyles. A small percentage of horses in the herd tend to harbor the majority of worms, and these horses are targeted for more frequent deworming.
Factors contributing to gastrointestinal parasitism in the horse are similar to those in other species: animal age; stocking density; geography and climate; presence and abundance of intermediate hosts; whether the animals are on pasture or dry lot; and pasture/paddock management practices.
Light parasite burdens are not associated with clinical disease, but heavy burdens can result in disease and death. Clinical signs of heavy parasitism include weight loss, stunted growth in juvenile horses, anemia and hypoproteinemia, colic (abdominal pain), acute or chronic diarrhea, and pulmonary injury. Young horses and immunodeficient geriatric horses are most susceptible to heavy parasite burdens and disease, but all horses are susceptible under the right conditions and in the absence of an effective parasite control program.
The goals of an equine parasite control program are to:
- Minimize the risk of parasite-related disease.
- Limit the extent of parasite shedding into the environment.
- Preserve the effectiveness of anti-parasitic medications.
As with vaccination programs, there is no such thing as a “one-size-fits-all” parasite control program that is appropriate for use in all horses!
Anti-Parasitic Medications
Over the past 30 years, widespread frequent use of over-the-counter oral anthelmintic products has resulted in excellent control of parasite-related disease across the population, but also accelerated the development of drug resistance among parasites. It was not uncommon to see that every horse on a farm was getting dewormed every 8 weeks, and often more frequently than that! In other words, too rigorous and indiscriminate an approach was taken. Resistance issues are of great concern because there are no new parasite control products in the drug production pipeline.
Current recommendations strive to avoid development of further resistance problems while still providing adequate protection from parasite-related disease. Compared to historical approaches, we now recommend a more strategic and targeted approach that results in much less frequent deworming for the majority of horses.
Horses are dewormed using over-the-counter commercial oral paste products that are dosed on the basis of body weight. Available medications include the macrocyclic lactones (ivermectin and moxidectin), pyrantel pamoate and tartrate, benzimidazoles (fenbendazole and oxibendazole), and praziquantel (available only in combination with ivermectin or moxidectin). To date, most parasite resistance is related to the benzimidazole and pyrantel products, but some resistance to the avermectins has also begun to appear recently. The parasite species most likely to exhibit resistance are small strongyles and ascarids.
A variety of herbal and organic deworming products are available and widely promoted among horse owners and managers, but there is no scientific evidence that these products are effective. They have not undergone formal testing for safety and efficacy, and are not approved or licensed as drugs by the FDA. Because non-drug products are allowed much more leniency in labeling, manufacturers can make almost any claim they want without having to substantiate that claim.
Design of Parasite Control Programs
In adult horses, decision-making about which horses to deworm, and with what products, is guided by serial quantitative fecal egg count (FEC) surveillance. Determination of the number of strongyle eggs per gram (epg) of manure helps owners and veterinarians to (i) estimate individual parasite burdens; (ii) identify the horses with moderate or heavy parasite burdens that will benefit from deworming; (iii) identify the specific horses within the herd that serve as the major long-term parasite reservoirs and require more frequent deworming; and (iv) determine which specific deworming products are effective against parasites on that farm.
On the basis of FEC, horses are categorized as low shedders (0-200 epg), moderate shedders (200-500 epg), or high shedders (> 500 epg). In a well managed herd it is common for 70-90% of adult horses to fall in the low-shedding category; these horses require as few as 2 deworming treatments per year (spring and fall). Management of moderate shedders varies by region, but these horses typically require at least one additional deworming treatment during the parasite transmission season. In Minnesota, for example, these horses generally receive one additional treatment for strongyles between April and October, with the timing dictated by the egg reappearance period (ERP) for the dewormer used in spring. Heavy shedders require treatment throughout the spring/summer parasite season, though never any earlier than the expected ERP for the deworming products used.
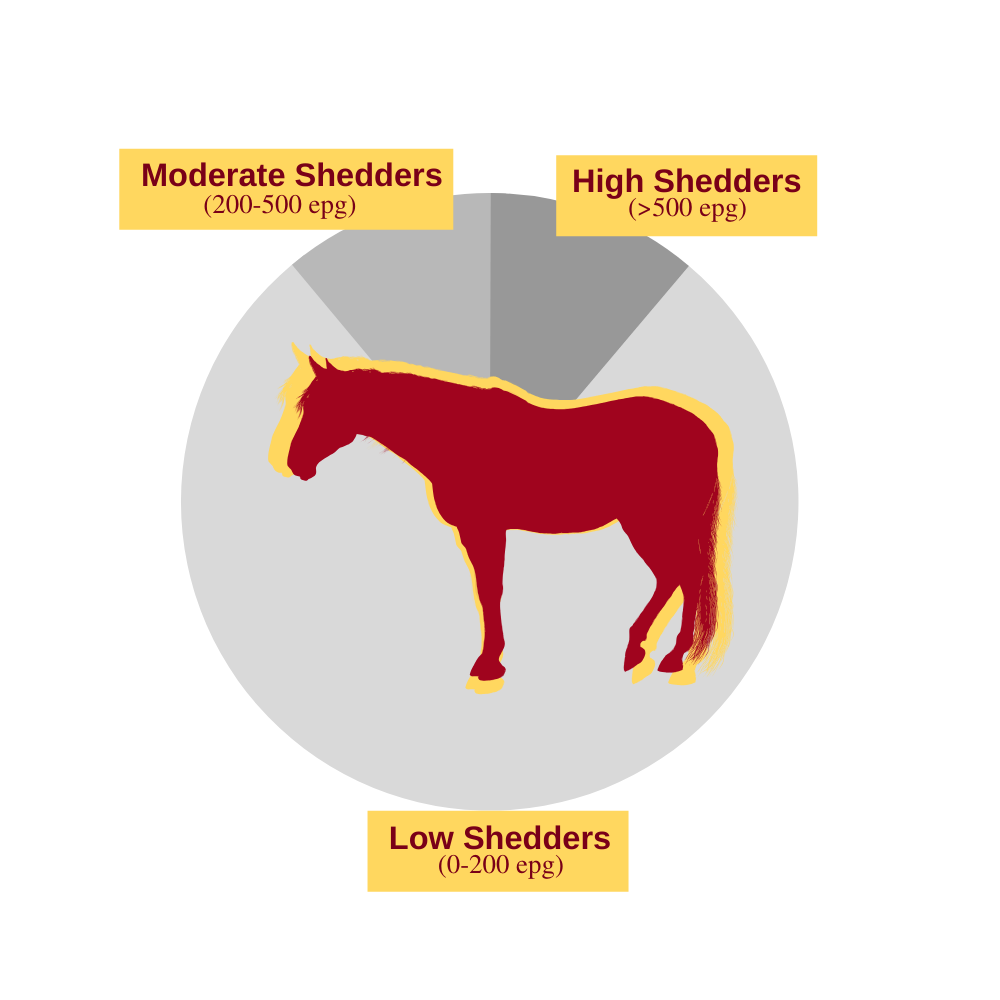
Fecal egg count reduction tests (FECRT) are used to evaluate the efficacy of specific deworming agents against both strongyles and ascarids. This entails running FEC tests immediately prior to worming and then 14 days after worming, and then calculating the percent reduction in fecal egg counts due to treatment. Specific cut-offs for suspicion of resistance vary between medications and parasites, but in general a dewormer should be dropping egg counts by 90-95% or more if the parasite is susceptible to its killing effects.
Under this type of program, adult horses with innate resistance to parasitism that carry low worm burdens are dewormed only 1-2 times per year. This ensures that many of the worms in the population are able to avoid the frequent exposure to deworming medications that selects for development of drug resistance. By contrast, horses with high worm burdens that are at greater risk for disease and contribute most to environmental contamination are selected for more frequent dosing. This applies some selection pressure for development of resistance, but is counterbalanced by the larger population of worms that remain genetically susceptible (refugia). The higher the proportion of worms in refugia, the more slowly resistance develops!
Foals, weanlings, and yearlings are approached differently due to their high level of susceptibility to parasitism in general, and ascarids in particular. Current recommendations are to treat them a minimum of 4 times in the first year of life, with the first treatment at 2-3 months of age using a benzimidazole (for example, fenbendazole). A second deworming is recommended just prior to weaning at approximately 6 months of age, prior to which an FEC is performed to determine whether worm burdens consist primarily of ascarids or of strongyles. The third and fourth treatments are administered at approximately 9 and 12 months of age, and should target primarily strongyles. One of those treatments should also include praziquantel to address tapeworms. Recently dewormed weanlings should be turned out into the cleanest pastures with the lowest worm/egg burdens.
Fecal egg counts are not useful for diagnosis of tapeworm or bot infestation, so most horses are simply treated annually for these in late fall on the assumption that a significant infestation exists. Praziquantel is the only medication licensed for treatment of tapeworms, while bots are treated with ivermectin or moxidectin. Timing this treatment for late in the fall serves to “clear out” the existing population of bots and tapeworms at a time when immediate reinfection is not possible because the flies and mites responsible for transmission are no longer active. Horses will begin to re-accumulate those parasites the following spring when flies and mites appear to resume transmission.
Environmental Management
As in other species, periodic administration of anthelmintic drugs is only one element of an effective control program and environmental sanitation and management are also important. The most effective approach is removal of manure from paddocks and pastures; twice-weekly manure collection is recommended. Dragging or harrowing paddocks and pastures to break up manure pats is much less effective, and only recommended for geographic regions in which spread manure will dry rapidly. Composting of manure and soiled bedding generates enough heat to kill parasite larvae and eggs. Non-composted manure should never be spread on pastures as this will serve to increase the level of parasite contamination. Reducing animal numbers, reducing stocking density, and avoiding overgrazing will reduce parasite exposure, as will rotating pastures and grazing other types of livestock on rested pastures. New horses should have an FEC on arrival, and be dewormed if warranted, before being turned out with resident horses.
*
 Small Animals
Small Animals
This is an excerpt from a book for pet owners (Root Kustritz MV (ed), The University of Minnesota Guide to Dog and Cat Wellness, ASIN: B00GCC0YN8).
Most puppies and kittens are born carrying some internal parasites, even if they are born into excellent breeding facilities. Your veterinarian can check the puppy or kitten’s feces for evidence of the parasites, but many infected puppies and kittens will test negative. Your veterinarian may recommend routine worming for your puppy or kitten several times when they are young, to ensure they are not carrying internal parasites. Adult dogs also may carry these parasites. If worm eggs in the feces hatch outside, the young worms may live in your lawn and infect humans, especially children, and other animals. Because of this, all feces should be picked up and disposed of immediately.
Intestinal parasites are treated with specific anti-parasitic drugs. *Note from Dr. Root for Preventive Medicine course – classes of wormers commonly used are those described for beef cattle (benzimidazoles and macrocyclic lactones) with some specific wormers for other classes used for things like tapeworms. Each type of worm is treated with a specific drug so it is important that the specific type of parasite present in your animal is identified. Over-the-counter wormers generally are not as effective as those available from your veterinarian. Some medications must be dosed more than once to destroy both juvenile and adult worms.
Heartworm is a form of internal parasite that infests the circulatory system. Young worms are injected by infected mosquitoes into the dog or cat. These young worms eventually lodge in the heart as adults where they mate and produce young worms that circulate in your dog or cat, infecting mosquitoes that feed on other animals and continuing the life cycle. Your dog or cat can contract heartworm anywhere they encounter mosquitoes, including indoors. The adult heartworms cause severe and potentially fatal damage to the heart, lungs, and other vital organs. Clinical signs of heartworm disease include coughing, fatigue, loss of appetite, and possibly episodes of fainting. Many infected dogs and cats show no signs of disease. Your veterinarian will test your dog yearly for this disorder; cats should be tested as well. Treatment is difficult so prevention is preferred. There is no treatment available for cats, so prevention is critical. Fortunately, cats are more resistant to heartworm disease than are dogs, so incidence of heartworm disease is lower in cats than in dogs. Your dog should be tested yearly and preventative medications given monthly. Heartworm preventive medications can be instituted in puppies as early as 6-8 weeks of age. Be aware that many heartworm medications also protect your pet against intestinal parasites described earlier.
*
Common Intestinal Parasites of Dogs and Cats
| COMMON NAME | APPEARANCE | CLINICAL SIGNS | HOW TRANSMITTED |
| Roundworms | 3-12″ long, spaghetti-like | Usually do not cause clinical signs; may see worms passed in feces, young animals may show poor weight gain. Most common in dogs and cats less than 6 months of age. | Eggs in feces, across the placenta or while nursing from the dam |
| Hookworms | Very small, thread-like | May see anemia, digested or frank blood in feces. | Eggs or young worms in feces, on the ground, nursing from the dam, penetration of larvae through skin |
| Whipworms | Very small, thread-like | Usually do not cause clinical signs; may occasionally be associated with diarrhea. | Eggs in feces, on the ground |
| Tapeworms | Very long and flat, made up of segments that look like grains of rice caught in the hair around the anus | May cause weight loss. | Eating rabbits, rodents, or eating fleas containing the worm. |
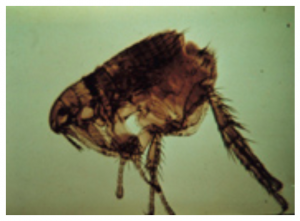
External parasites of most concern are ticks and fleas. Fleas feed on blood and can transmit disease, including tapeworms. Fleas are primarily an environmental concern; 95% of the flea population (eggs, larvae and pupae) live in the environment and only 5% (adult) live on animals. Outside areas exposed to sunlight in summer or extreme cold in winter are unlikely to harbor fleas. Inside the home, flea populations will be concentrated where the animal spends the most time resting or sleeping. Fleas are the most common external parasite in small animals; cats are twice as likely as dogs to have fleas when examined by veterinarians. Successful flea control requires treatment of the animal and the environment. There are excellent flea control products available. Not all are safe for use in puppies and kittens.
Ticks can transmit disease to dogs including Lyme disease, anaplasmosis, ehrlichiosis, and Rocky Mountain Spotted Fever. Safe and effective tick products are available but there is no tick preventative that is 100% effective; dogs and outside cats should be checked and ticks removed by hand at least once daily in the warmer months.

Fleas and Ticks in Small Animals
 |
 |
 |
 |
 |
*
Control of small animal parasites in shelter / rescue operations
It is estimated that as many as 40% of owned dogs and cats in the United States have been through some sort of animal shelter. Animals entering shelters may be in poor condition and are closely housed, which increases risk of exposure. Many internal parasites release eggs or cysts that are impervious to disinfecting agents. Shelters must be rigorous about prompt removal of feces and regular complete cleaning of facilities to decrease overall exposure. Animals commonly are treated with appropriate medications for control of roundworms, hookworms, whipworms, and coccidia, with repeated treatment every 2 weeks if needed.
 Extra Resources
Extra Resources
- Flea products: https://todaysveterinarypractice.com/practical-parasitologythe-flea-infested-pet-overview-current-products/
- Managing fleas on the pet and in the environment: https://todaysveterinarypractice.com/practical-parasitologythe-flea-infested-pethow-manage-pet-environment/
- Fly control products and approvals: http://entomology.unl.edu/livestock
- Applicability of the Antiparasitic Resistance Management Strategy (ARMS) to cattle: https://www.fda.gov/animal-veterinary/safety-health/antiparasitic-resistance
- American Consortium for Small Ruminant Parasite Control: www.acsrpc.org
- Internal parasite categories in swine: https://thepigsite.com/disease-guide/endoparasites-internal-parasites-worms-nematodes
- External parasite categories in swine: https://thepigsite.com/disease-guide/ectoparasites
- Fleas in small animals: https://www.banfield.com/state-of-pet-health/skin-allergies/overview