104 Prevention and Treatment of Viral Infections
- Identify major viral illnesses that affect humans
- Compare vaccinations and anti-viral drugs as medical approaches to viruses
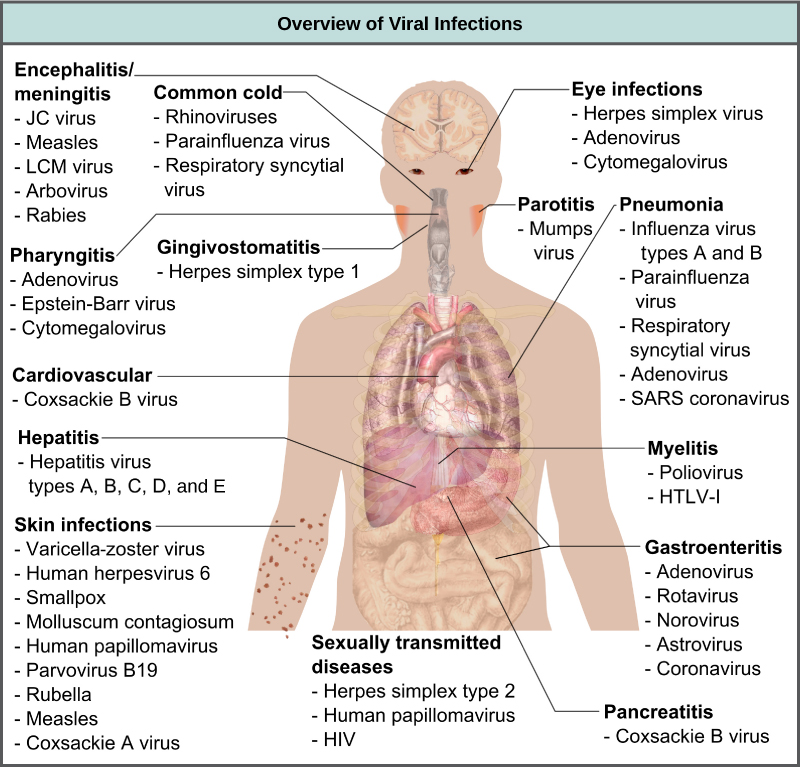
Viruses cause a variety of diseases in animals, including humans, ranging from the common cold to potentially fatal illnesses like meningitis (Figure 1). These diseases can be treated by antiviral drugs or by vaccines; however, some viruses, such as HIV, are capable both of avoiding the immune response and of mutating within the host organism to become resistant to antiviral drugs.
Vaccines for Prevention
The primary method of controlling viral disease is by vaccination, which is intended to prevent outbreaks by building immunity to a virus or virus family (Figure 2). Vaccines may be prepared using live viruses, killed viruses, or molecular subunits of the virus. Note that the killed viral vaccines and subunit viruses are both incapable of causing disease, nor is there any valid evidence that vaccinations contribute to autism.
Live viral vaccines are designed in the laboratory to cause few symptoms in recipients while giving them protective immunity against future infections. Polio was one disease that represented a milestone in the use of vaccines. Mass immunization campaigns in the 1950s (killed vaccine) and 1960s (live vaccine) significantly reduced the incidence of the disease, which caused muscle paralysis in children and generated a great amount of fear in the general population when regional epidemics occurred. The success of the polio vaccine paved the way for the routine dispensation of childhood vaccines against measles, mumps, rubella, chickenpox, and other diseases.
The issue with using live vaccines (which are usually more effective than killed vaccines), is the low but significant danger that these viruses will revert to their disease-causing form by back mutations. Live vaccines are usually made by attenuating (weakening) the “wild-type” (disease-causing) virus by growing it in the laboratory in tissues or at temperatures different from what the virus is accustomed to in the host. Adaptations to these new cells or temperatures induce mutations in the genomes of the virus, allowing it to grow better in the laboratory while inhibiting its ability to cause disease when reintroduced into conditions found in the host. These attenuated viruses thus still cause infection, but they do not grow very well, allowing the immune response to develop in time to prevent major disease. Back mutations occur when the vaccine undergoes mutations in the host such that it readapts to the host and can again cause disease, which can then be spread to other humans in an epidemic. This type of scenario happened as recently as 2007 in Nigeria where mutations in a polio vaccine led to an epidemic of polio in that country.
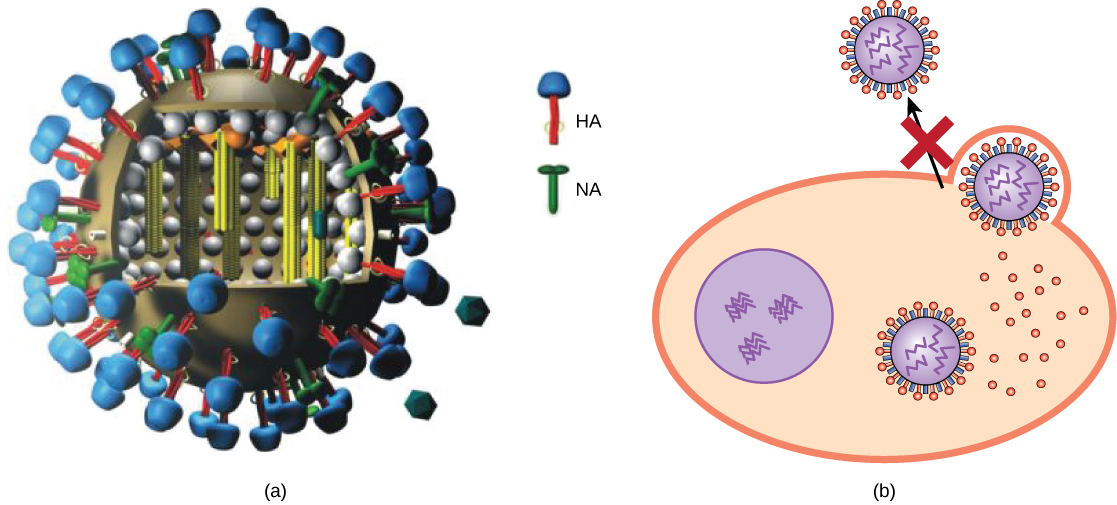
Some vaccines are in continuous development because certain viruses, such as influenza and HIV, have a high mutation rate compared to that of other viruses and normal host cells. With influenza, mutations in the surface molecules of the virus help the organism evade the protective immunity that may have been obtained in a previous influenza season, making it necessary for individuals to get vaccinated every year. Other viruses, such as those that cause the childhood diseases measles, mumps, and rubella, mutate so infrequently that the same vaccine is used year after year.

LINK TO LEARNING
Watch this NOVA video to learn how microbiologists are attempting to replicate the deadly 1918 Spanish influenza virus so they can understand more about virology.
Vaccines and Antiviral Drugs for Treatment
In some cases, vaccines can be used to treat an active viral infection. The concept behind this is that by giving the vaccine, immunity is boosted without adding more disease-causing virus. In the case of rabies, a fatal neurological disease transmitted via the saliva of rabies virus-infected animals, the progression of the disease from the time of the animal bite to the time it enters the central nervous system may be two weeks or longer. This is enough time to vaccinate individuals who suspect that they have been bitten by a rabid animal, and their boosted immune response is sufficient to prevent the virus from entering nervous tissue. Thus, the potentially fatal neurological consequences of the disease are averted, and the individual only has to recover from the infected bite. This approach is also being used for the treatment of Ebola, one of the fastest and most deadly viruses on Earth. Transmitted by bats and great apes, this disease can cause death in 70 to 90 percent of infected humans within two weeks. Using newly developed vaccines that boost the immune response in this way, there is hope that affected individuals will be better able to control the virus, potentially saving a greater percentage of infected persons from a rapid and very painful death.
Another way of treating viral infections is the use of antiviral drugs. Because viruses use the resources of the host cell for replication and the production of new virus proteins, it is difficult to block their activities without damaging the host. However, we do have some effective antiviral drugs, such as those used to treat HIV and influenza. Some antiviral drugs are specific for a particular virus and others have been used to control and reduce symptoms for a wide variety of viral diseases. For most viruses, these drugs can inhibit the virus by blocking the actions of one or more of its proteins. It is important to note that the targeted proteins be encoded by viral genes and that these molecules are not present in a healthy host cell. In this way, viral growth is inhibited without damaging the host.
Antivirals have been developed to treat genital herpes (herpes simplex II) and influenza. For genital herpes, drugs such as acyclovir can reduce the number and duration of episodes of active viral disease, during which patients develop viral lesions in their skin cells. As the virus remains latent in nervous tissue of the body for life, this drug is not curative but can make the symptoms of the disease more manageable. For influenza, drugs like Tamiflu (oseltamivir) (Figure 3) can reduce the duration of “flu” symptoms by one or two days, but the drug does not prevent symptoms entirely. Tamiflu works by inhibiting an enzyme (viral neuraminidase) that allows new virions to leave their infected cells. Thus, Tamiflu inhibits the spread of virus from infected to uninfected cells. Other antiviral drugs, such as Ribavirin, have been used to treat a variety of viral infections, although its mechanism of action against certain viruses remains unclear.
By far, the most successful use of antivirals has been in the treatment of the retrovirus HIV, which causes a disease that, if untreated, is usually fatal within 10 to 12 years after infection. Anti-HIV drugs have been able to control viral replication to the point that individuals receiving these drugs survive for a significantly longer time than the untreated.
Anti-HIV drugs inhibit viral replication at many different phases of the HIV replicative cycle (Figure 4). Drugs have been developed that inhibit the fusion of the HIV viral envelope with the plasma membrane of the host cell (fusion inhibitors), the conversion of its RNA genome into double-stranded DNA (reverse transcriptase inhibitors, like AZT), the integration of the viral DNA into the host genome (integrase inhibitors), and the processing of viral proteins (protease inhibitors).
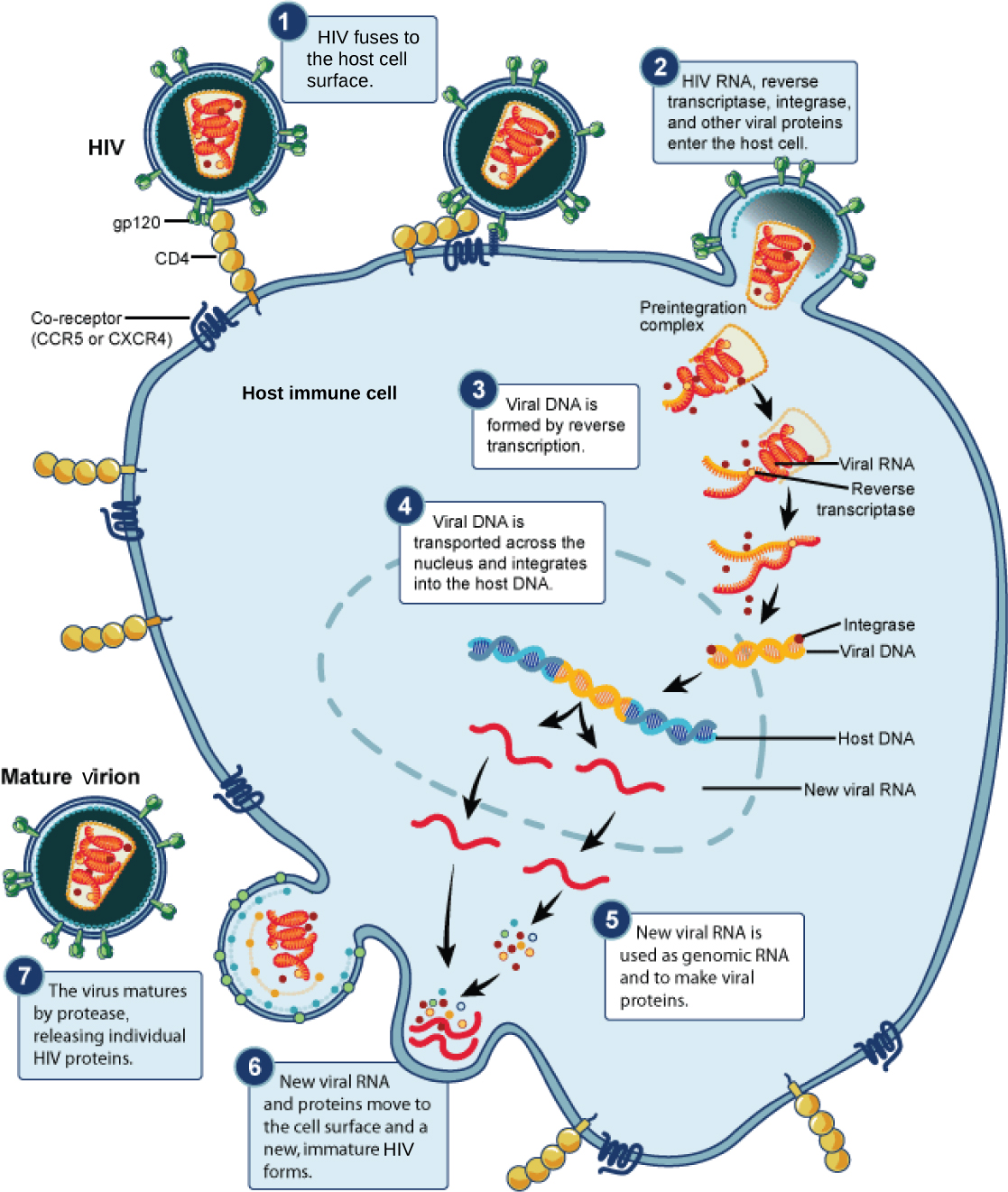
Unfortunately, when any of these drugs are used individually, the high mutation rate of the virus allows it to easily and rapidly develop resistance to the drug, limiting the drug’s effectiveness. The breakthrough in the treatment of HIV was the development of HAART, highly active anti-retroviral therapy, which involves a mixture of different drugs, sometimes called a drug “cocktail.” By attacking the virus at different stages of its replicative cycle, it is much more difficult for the virus to develop resistance to multiple drugs at the same time. Still, even with the use of combination HAART therapy, there is concern that, over time, the virus will develop resistance to this therapy. Thus, new anti-HIV drugs are constantly being developed with the hope of continuing the battle against this highly fatal virus.
EVERYDAY CONNECTION
Applied Virology
The study of viruses has led to the development of a variety of new ways to treat non-viral diseases. Viruses have been used in gene therapy. Gene therapy is used to treat genetic diseases such as severe combined immunodeficiency (SCID), a heritable, recessive disease in which children are born with severely compromised immune systems. One common type of SCID is due to the lack of an enzyme, adenosine deaminase (ADA), which breaks down purine bases. To treat this disease by gene therapy, bone marrow cells are taken from a SCID patient and the ADA gene is inserted. This is where viruses come in, and their use relies on their ability to penetrate living cells and bring genes in with them. Viruses such as adenovirus, an upper-respiratory human virus, are modified by the addition of the ADA gene, and the virus then transports this gene into the cell. The modified cells, now capable of making ADA, are then given back to the patients in the hope of curing them. Gene therapy using viruses as carriers of genes (viral vectors), although still experimental, holds promise for the treatment of many genetic diseases. Still, many technological problems need to be solved for this approach to be a viable method for treating genetic disease.
Another medical use for viruses relies on their specificity and ability to kill the cells they infect. Oncolytic viruses are engineered in the laboratory specifically to attack and kill cancer cells. A genetically modified adenovirus known as H101 has been used since 2005 in clinical trials in China to treat head and neck cancers. The results have been promising, with a greater short-term response rate to the combination of chemotherapy and viral therapy than to chemotherapy treatment alone. This ongoing research may herald the beginning of a new age of cancer therapy, where viruses are engineered to find and specifically kill cancer cells, regardless of where in the body they may have spread.
A third use of viruses in medicine relies on their specificity and involves using bacteriophages in the treatment of bacterial infections. Bacterial diseases have been treated with antibiotics since the 1940s. However, over time, many bacteria have evolved resistance to antibiotics. A good example is methicillin-resistant Staphylococcus aureus (MRSA, pronounced “mersa”), an infection commonly acquired in hospitals. This bacterium is resistant to a variety of antibiotics, making it difficult to treat. The use of bacteriophages specific for such bacteria would bypass their resistance to antibiotics and specifically kill them. Although phage therapy is in use in the Republic of Georgia to treat antibiotic-resistant bacteria, its use to treat human diseases has not been approved in most countries. However, the safety of the treatment was confirmed in the United States when the U.S. Food and Drug Administration approved spraying meats with bacteriophages to destroy the food pathogen Listeria. As more and more antibiotic-resistant strains of bacteria evolve, the use of bacteriophages might be a potential solution to the problem, and the development of phage therapy is of much interest to researchers worldwide.
- attenuation
- weakening of a virus during vaccine development
- back mutation
- when a live virus vaccine reverts back to it disease-causing phenotype
- gene therapy
- treatment of genetic disease by adding genes, using viruses to carry the new genes inside the cell
- oncolytic virus
- virus engineered to specifically infect and kill cancer cells
- phage therapy
- treatment of bacterial diseases using bacteriophages specific to a particular bacterium
- vaccine
- weakened solution of virus components, viruses, or other agents that produce an immune response
