100 Adaptation in Humans
GOT LACTASE?
Do you remember this “got milk?” slogan from the 1990s? It was used in ads for milk in which celebrities were pictured wearing milk “mustaches.” While the purpose of the “got milk?” ads was to sell more milk, there is no denying that drinking milk can be good for one’s health. Milk is naturally high in protein and minerals. It can also be low in fat or even fat-free if treated to remove the lipids that naturally occur in milk. However, before you reach for a tall, cold glass of milk, you might want to ask yourself another question: “got lactase?”

Adaptation to Lactose
Do you drink milk? Or do you avoid drinking milk and consuming milk products because they cause you discomfort? If the latter is the case, then you may have trouble digesting milk.
Milk, Lactose, and Lactase
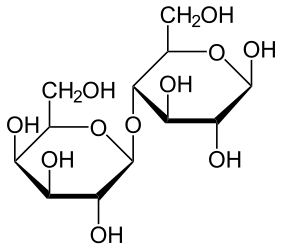
Milk naturally contains not only proteins and lipids; it also contains carbohydrates. Specifically, milk contains the sugar lactose. Lactose is a disaccharide (two-sugar) compound that consists of one molecule each of galactose and glucose, as shown in the structural formula below. Lactose makes up between 2 and 8 percent of milk by weight. The exact amount varies both within and between species.
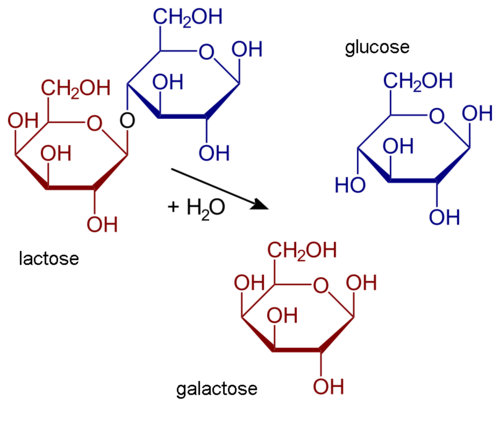
Lactose in milk must be broken down into its two component sugars to be absorbed by the small intestine. The enzyme lactase is needed for this process, as shown in the diagram below. Human infants are almost always born with the ability to synthesize lactase. This allows them to readily digest the lactose in their mother’s milk (or in infant formula). However, in the majority of infants, lactase synthesis begins to decline at about 2 years of age, and less and less lactase is produced throughout childhood.
Lactose intolerance is the inability of older children and adults to digest lactose in milk. People who are lactose intolerant may be able to drink small quantities of milk without any problems, but if they try to consume larger amounts, they are likely to suffer adverse effects. For example, they may have abdominal bloating and cramping, flatulence (gas), diarrhea, nausea, and vomiting. The symptoms may occur from one-half to two hours after milk is consumed and are generally worse when the quantity of milk consumed is greater. The symptoms result from the inability of the small intestine to digest and absorb lactose, so the lactose is passed on to the large intestine, where normal intestinal bacteria start breaking it down through the process of fermentation. This process releases gas and causes other symptoms of lactose intolerance.
Lactose intolerance is actually the original and normal condition of the human species, as it is of all other mammalian species. Early humans were hunter-gatherers that subsisted on wild plant and animal foods. The animal foods may have included meat and eggs but did not include milk because animals had not been domesticated. Therefore, beyond the weaning period, milk was not available for people to drink in early human populations. It makes good biological sense to stop synthesizing an enzyme that the body does not need. After a young child is weaned, it is a waste of materials and energy to keep producing lactase when milk is no longer likely to be consumed.
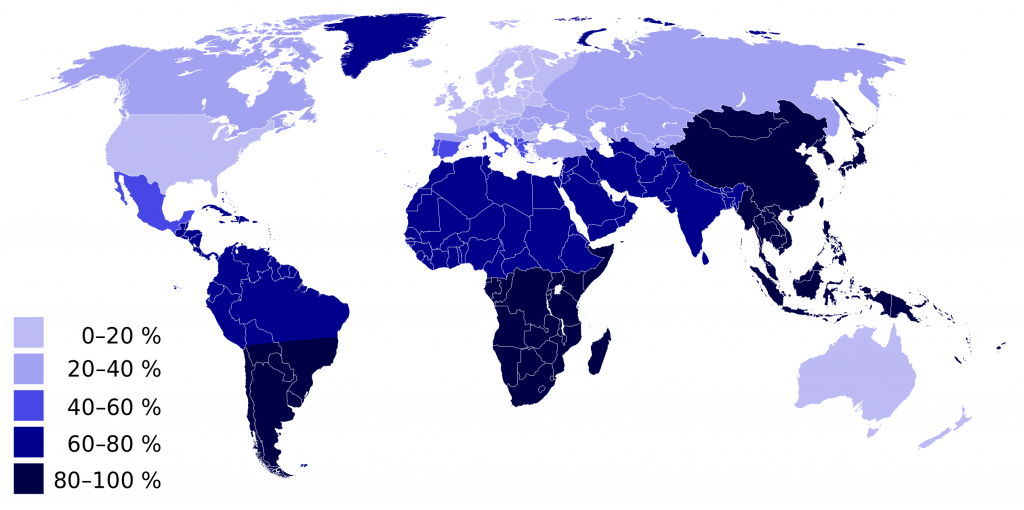
Overall, an estimated 60 percent of the world’s adult human population is thought to be lactose intolerant today. You can see the geographic distribution of modern human lactose intolerance on the map above (Figure 4). Lactose intolerance (Figure 4, dark blue) approaches 100 percent in populations throughout southern South America, southern Africa, and East and Southeast Asia.
Lactose intolerance is not considered to be a medical problem because its symptoms can be avoided by not consuming milk or milk products. Dietary control of lactose intolerance may be a matter of trial and error, however, because different people may be able to consume different quantities of milk before symptoms occur. If you are lactose intolerant, be aware that low-fat and fat-free milk may contain somewhat more lactose than full-fat milk because the former often have added milk solids that are relatively high in lactose.
Lactase Persistence

Lactase persistence is the opposite of lactose intolerance. People who are lactase persistent continue to produce the enzyme lactase beyond infancy and generally throughout life. As a consequence, they are able to digest lactose and drink milk at older ages without adverse effects. The map above (Figure 4) can also be read to show where lactase persistence occurs today. Populations with a low percentage of lactose intolerance (including most North Americans and Western and Northern Europeans) have high percentages of lactase-persistent people.
Lactase persistence is a uniquely human trait that is not found in any other mammalian species. Why did lactase persistence evolve in humans? When some human populations began domesticating and keeping herds of animals, animal milk became a potential source of food. Animals such as cows, sheep, goats, camels, and even reindeer (Figure 5) can be kept for their milk. These kinds of animal milk also contain lactose, so natural selection would be strong for any individuals who kept producing lactase beyond infancy and could make use of this nutritious food. Eventually, the trait of lactase persistence would increase in frequency and come to be the predominant trait in dairying populations.
It is likely that lactase persistence occurs as a result of both genes and environment. Some people inherit genes that help them keep producing lactase after infancy. Geneticists think that several different mutations for lactase persistence arose independently in different populations within the last 10,000 years. Part of lactase persistence may be due to continued exposure to milk in the diet in childhood and adulthood. In other words, a person may be genetically predisposed to synthesize lactase at older ages because of a mutation but may need the continued stimulation of milk drinking to keep producing lactase.
Thrifty Gene or Drifty Gene?
Besides variation in lactase persistence, human populations may vary in how efficiently they use calories in the foods they consume. People in some populations seem to be able to get by on quantities of food that would be inadequate for others, so they tend to gain weight easily. What explains these differences in people?
Thrifty Gene Hypothesis
In 1962, human geneticist James Neel proposed the thrifty gene hypothesis. According to this hypothesis, so-called “thrifty genes” evolved in some human populations because they allowed people to get by on fewer calories and store the rest as body fat when food was plentiful. According to Neel’s hypothesis, thrifty genes would have increased in frequency through natural selection because they would help people survive during times of famine. People with the genes would be fatter and able to rely on their stored body fat for calories when food was scarce.
Such thrifty genes would have been advantageous in early human populations of hunter-gathers if food scarcity was a recurrent stress. However, in modern times, when most people have access to enough food year-round, thrifty genes would no longer be advantageous. In fact, under conditions of plentiful food, having thrifty genes would predispose people to gain weight and develop obesity. They would also tend to develop a chronic disease associated with obesity, particularly type II diabetes. Diabetes mellitus is a disease that occurs when there are problems with the pancreatic hormone insulin, which normally helps cells take up glucose from the blood and controls blood glucose levels. In type II diabetes, body cells become relatively resistant to insulin, leading to high blood glucose. This causes symptoms including excessive thirst and urination. Without treatment, diabetes can lead to serious consequences, such as blindness and kidney failure.
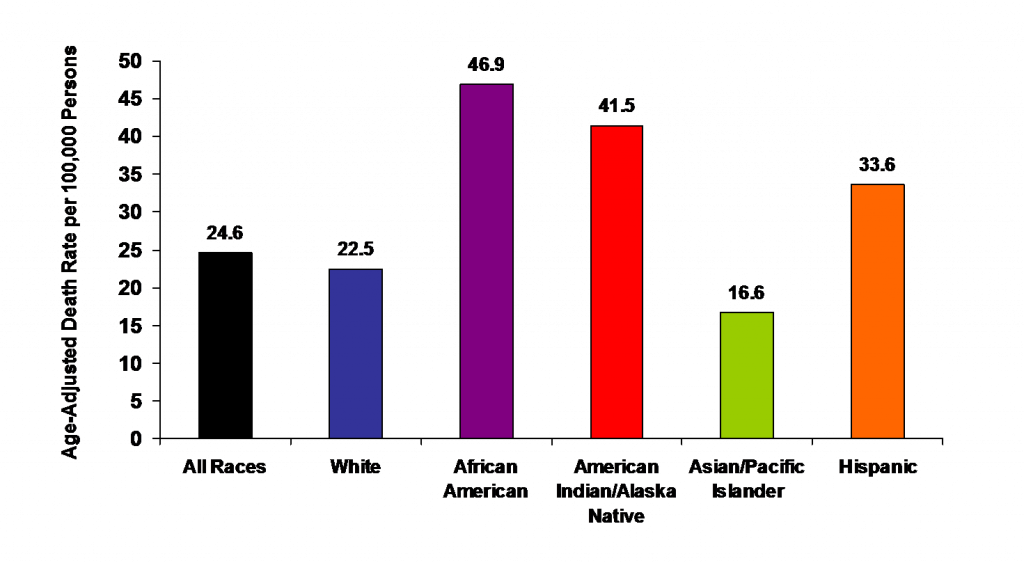
Neel proposed his thrifty gene hypothesis not on the basis of genetic evidence for thrifty genes but as a possible answer to the mystery of why genes that seem to promote diabetes have not been naturally selected out of some populations. The mystery arose from observations that certain populations — such as South Pacific Islanders, sub-Saharan Africans, and southwestern Native Americans — developed high levels of obesity and diabetes after they abandoned traditional diets and adopted Western diets. This is reflected in the 2005 death rates from diabetes in the U.S. population, as shown in the graph below (Figure 6). The single largest group in the U.S. population is the “white” group, but they had the second lowest number of diabetes deaths. Death rates from diabetes were disproportionately high in the other ethnic groups, especially those with African or Native American ancestry.
Assessing the Thrifty Gene Hypothesis
One of the assumptions underlying the thrifty gene hypothesis is that human populations that recently developed high rates of obesity and diabetes after Western contact had a long history of recurrent famine. Anthropological evidence contradicts this assumption for at least some of the populations in question. For example, South Pacific Islanders have long lived in a “land of plenty,” with lush tropical forests year-round on islands surrounded by warm waters full of fish. Another assumption underlying the thrifty gene hypothesis is that hunter-gatherer people became significantly fatter during periods of plenty. Again, there is little or no evidence that hunter-gatherers traditionally deposited large fat stores when food was readily available.
Some geneticists have searched directly for so-called thrifty genes. Studies have revealed many genes with small effects associated with obesity or diabetes. However, these genes can explain only a few percentage points of the total population variation in obesity or diabetes.
The Drifty Gene and Other Hypotheses
Given the lack of evidence for the thrifty gene hypothesis, several researchers have suggested alternative hypotheses to explain population variation in obesity and diabetes. One hypothesis posits that susceptibility to obesity and diabetes may be a side effect of heat adaptation. According to this idea, some populations evolved lower metabolic rates as an adaptation to heat stress, because lower metabolic rates reduced the amount of heat that the body produced. The lower metabolic rates also predisposed people to gain excess weight and develop obesity and diabetes.
A thrifty phenotype hypothesis has also been proposed. This hypothesis suggests that individuals who have inadequate nutrition during fetal development might develop an insulin-resistant phenotype. The insulin-resistant phenotype would supposedly prepare these individuals for a life of famine, based on the environment within the womb. In a famine-free environment, however, the thrifty phenotype would lead to the development of diabetes.
The most recent alternative to the thrifty gene hypothesis is the drifty gene hypothesis proposed by biologist John Speakman. He argues that genes protecting humans from obesity were under strong natural selection pressure for a very long period of time while human ancestors were subject to the risk of predation. According to this view, being able to outrun predators would have been an important factor selecting against fatness. When the risk of predation was lessened, perhaps as early as 2 million years ago, genes keeping fatness in check would no longer be selected for. Without selective pressure for these genes, their frequencies could change randomly due to genetic drift. In some populations, by chance, frequencies of the genes could decrease to relatively low levels, whereas in other populations the frequencies could be much higher.
FEATURE: MYTH VS. REALITY
Myth: Lactose intolerance is an allergy to milk.
Reality: Lactose intolerance is not an allergy because it is not an immune system response. Rather, it is a sensitivity to milk that is caused by lactase deficiency so the sugar in milk cannot be digested. Milk allergy does exist, but it is a different condition that occurs in only about 4 percent of people. It results when milk proteins (not milk sugar) trigger an immune reaction. How can you determine whether you have lactose intolerance or milk allergy? If you can drink lactose-free milk without symptoms, it is likely that you are lactose intolerant and not allergic to milk. However, if lactose-free milk also produces symptoms, it is likely that you have milk allergy. Note that it is possible to have both conditions.
Myth: If you are lactose intolerant, you will never be able to drink milk or consume other dairy products without suffering adverse physical symptoms.
Reality: Lactose intolerance does not mean that consuming milk and other dairy products is out of the question. Besides lactose-free milk, which is widely available, many dairy products have relatively low levels of lactose, so you may be able to consume at least small amounts of them without discomfort. For example, you may be able to consume milk in the form of yogurt without any problems because the bacteria in yogurt produce lactase that breaks down the lactose. Greek yogurt may be your best bet because it is lower in lactose to begin with. Aged cheeses also tend to have relatively low levels of lactose because of the cheese-making process. Finally, by gradually adding milk or milk products to your diet, you may be able to increase your tolerance to lactose.
EXPLORE MORE
Does obesity lead to diabetes, or could it be the other way around? Hear a provocative answer to this question in this moving TED talk.
This chapter by Suzanne Wakim & Mandeep Grewal is licensed CC BY-SA 4.0.

