Somatosensation
10 Overview of Somatosensation
Learning Objectives
Know that somatosensation includes touch (mechanical and thermal), pain (mechanical, thermal, chemical) & proprioception (sense of self—the topic of the next chapter).
Know the primary categories of cutaneous senses: mechanical, thermal, and noxious.
Somatosensation (Touch)
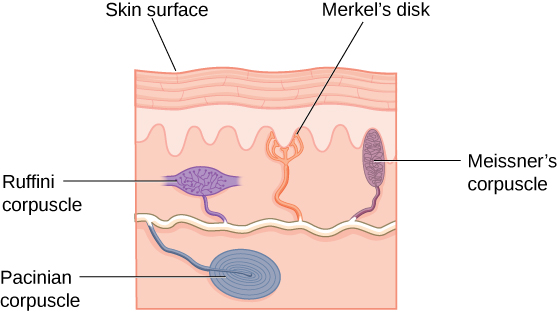
Somatosensation is considered a general sense, as opposed to the special senses discussed in this section. Somatosensation is the group of sensory modalities that are associated with touch, proprioception, and interoception. These modalities include pressure, vibration, light touch, tickle, itch, temperature, pain, proprioception, and kinesthesia. This means that its receptors are not associated with a specialized organ, but are instead spread throughout the body in a variety of organs (Fig.2.1.1). Many of the somatosensory receptors are located in the skin, but receptors are also found in muscles, tendons, joint capsules, ligaments, and in the walls of visceral organs.
Two types of somatosensory signals that are transduced by free nerve endings are pain and temperature. These two modalities use thermoreceptors and nociceptors to transduce temperature and pain stimuli, respectively. Temperature receptors are stimulated when local temperatures differ from body temperature. Some thermoreceptors are sensitive to just cold and others to just heat. Nociception is the sensation of potentially damaging stimuli. Mechanical, chemical, or thermal stimuli beyond a set threshold will elicit painful sensations. Stressed or damaged tissues release chemicals that activate receptor proteins in the nociceptors. For example, the sensation of heat associated with spicy foods involves capsaicin, the active molecule in hot peppers. Capsaicin molecules bind to a transmembrane ion channel in nociceptors that is sensitive to temperatures above 37°C. The dynamics of capsaicin binding with this transmembrane ion channel is unusual in that the molecule remains bound for a long time. Because of this, it will decrease the ability of other stimuli to elicit pain sensations through the activated nociceptor. For this reason, capsaicin can be used as a topical analgesic, such as in products such as Icy Hot™.
If you drag your finger across a textured surface, the skin on your finger will vibrate. Such low frequency vibrations are sensed by mechanoreceptors called Merkel cells (figure x), also known as type I cutaneous mechanoreceptors. Merkel cells are located in the stratum basale of the epidermis. Deep pressure and vibration is transduced by lamellated (Pacinian) corpuscles, which are receptors with encapsulated endings found deep in the dermis, or subcutaneous tissue. Light touch is transduced by the encapsulated endings known as tactile (Meissner) corpuscles. Follicles are also wrapped in a plexus of nerve endings known as the hair follicle plexus. These nerve endings detect the movement of hair at the surface of the skin, such as when an insect may be walking along the skin. Stretching of the skin is transduced by stretch receptors known as bulbous corpuscles. Bulbous corpuscles are also known as Ruffini corpuscles, or type II cutaneous mechanoreceptors.
Other somatosensory receptors are found in the joints and muscles. Stretch receptors monitor the stretching of tendons, muscles, and the components of joints. For example, have you ever stretched your muscles before or after exercise and noticed that you can only stretch so far before your muscles spasm back to a less stretched state? This spasm is a reflex that is initiated by stretch receptors to avoid muscle tearing. Such stretch receptors can also prevent over-contraction of a muscle. In skeletal muscle tissue, these stretch receptors are called muscle spindles. Golgi tendon organs similarly transduce the stretch levels of tendons. Bulbous corpuscles are also present in joint capsules, where they measure stretch in the components of the skeletal system within the joint.
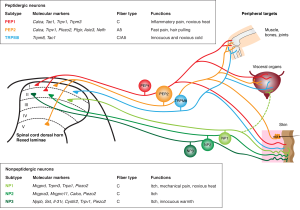
Most of your non-proprioceptive somatosensory neurons are cutaneous sensory neurons in your skin. They fall into 3 categories: Mechanical, Thermal, and Noxious. Most cutaneous receptors are pseudo-unipolar neurons, with cell bodies in the dorsal root ganglia. The dorsal root ganglia (singular: ganglion; plural: ganglia) are lumps of nervous tissue next to the spinal cord that house the cell bodies of somatosensory neurons.
Primary somatosensory neurons can transduce various thermal and nociceptive stimuli into action potentials that propagate toward the central nervous system (Raoux et al., 2007; licensed CC-BY-PDM 1.0). Most of these sensory neurons are also responsive to some forms of mechanical stimuli and as such function as mechanoreceptors. The mechanical stimulation of these mechanoreceptors generates a variety of sensations, such as touch, pressure, vibration, proprioception, and pain. Sensory ganglia contain both low threshold mechanoreceptors (LTMs), which respond to light touch, vibration, or internally generated movements, and high threshold mechanoreceptors (HTMs or mechanonociceptors) which sense noxious levels of pressure.
Tiny stimulation spots evoke discrete cold or touch percepts, and more recent afferent ablation studies alter percepts of specific modalities, it has been suggested that the circuits carrying thermal information are anatomically distinct from touch, pain, and proprioception — a ‘labeled line’ system (Bokiniec et al., 2018; license CC BY-NC-ND). However, the perception of cold and warm co-varies in humans, and multi-modal (mostly touch and temperature) responses have been observed at the afferent, thalamic, and cortical levels of the thermal system.
Pain and itch are sensory mechanisms essential for protecting the body from potentially harmful external agents (Cranfill & Luo, 2021; licensed CC-BY-PDM 1.0). Although pain and itch elicit distinct sensory experiences and behavioral responses – rubbing/withdrawal for pain, and scratching for itch – there is extensive overlap in the neurons and circuits mediating these sensations. Both noxious and pruriceptive (itchy) stimuli are detected by specialized sensory neurons of the dorsal root ganglia (DRG) and trigeminal ganglia (TG) called nociceptors, of which pruriceptors are a subset.
A variety of noxious stimuli and functions downstream of sensory G-protein coupled receptors (GPCRs), and the Mas-related GPCR family (MRGPRs), transduce a wide variety of endogenous and exogenous itch signals. Other important receptor types implicated in itch include histamine receptors, serotonin receptors, cytokine receptors, and toll-like receptors.
To review the different types of receptors, you can watch this seven minute Khan Academy video linked here and included below.
CC LICENSED CONTENT, SHARED PREVIOUSLY
OpenStax, Anatomy and Physiology Chapter 14.1 Sensory Perception
Provided by: Rice University.
Access for free at https://openstax.org/books/anatomy-and-physiology/pages/14-1-sensory-perception
License: CC-BY 4.0
Cheryl Olman PSY 3031 Detailed Outline
Provided by: University of Minnesota
Download for free at http://vision.psych.umn.edu/users/caolman/courses/PSY3031/
License of original source: CC Attribution 4.0
Adapted by: Avery Bennett
Bokiniec, P., Zampieri, N., Lewin, G. R., & Poulet, J. F. (2018). The neural circuits of thermal perception. Current Opinion in Neurobiology, 52, 98-106. https://doi.org/10.1016/j.conb.2018.04.006
Cranfill, S. L., & Luo, W. (2021). The Development of Somatosensory Neurons: Insights into Pain and Itch. Current Topics in Developmental Biology, 142, 443. https://doi.org/10.1016/bs.ctdb.2020.10.005
Raoux, M., Rodat-Despoix, L., Azorin, N., Giamarchi, A., Hao, J., Maingret, F., Crest, M., Coste, B., & Delmas, P. (2007). Mechanosensor Channels in Mammalian Somatosensory Neurons. Sensors (Basel, Switzerland), 7(9), 1667-1682. https://doi.org/10.3390/s7091667

