Vision Loss and V1
97 Visual Prosthetics
Learning Objectives
Know how retinal and cortical implants work.
Know what the requirements are for a retinal and cortical implants.
Know what the limitations of current retinal and cortical implants are.
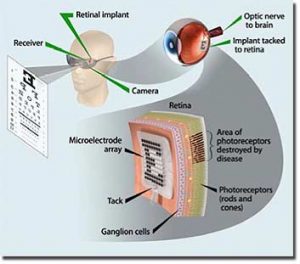
Retinal implants take images from an external video camera which sends electric signals to an array implanted in the eye, bypassing damaged photoreceptors to kick-start retinal cells that are still viable. Minimally, a patient must have an intact ganglion cell layer in order to be a candidate for a retinal implant. Optimal candidates for retinal implants have retinal diseases, such as retinitis pigmentosa or age-related macular degeneration. Other factors, including amount of residual vision, overall health, and family commitment to rehabilitation, are also considered when determining candidates for retinal implants.
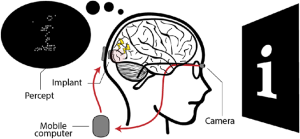
A cortical implant is a subset of neuroprosthetics that is in direct connection with the cerebral cortex of the brain. Certain types of cortical implants can partially restore vision by directly stimulating the visual cortex. Cortical visual prostheses are important to people who have a completely damaged retina, optic nerve, or lateral geniculate body, as they are one of the only ways they would be able to have their vision restored.
Limitations to the implants
Both prosthetic solutions have a resolution problem: to provide even low vision, we would need to stimulate neurons with a spatial precision of 100 microns, and right now, the precision is measured in millimeters. So the current goal is to restore useful visual experiences to people who have none. Both approaches share the problems of biocompatibility and stability: the salt-water environment of the body is hostile to electronics, and scar tissue degrades performance of devices over time.
Retinal implants need to contend with the fact that the eye moves rapidly and the retinal sheet is delicate. Cortical implants have more neural territory to work with, but permanent brain implants bring risks of infection, inflammation, and other complications you don’t want in your brain.
Argus and Orion prosthetics
The Argus II, developed by Second Sight with NEI support, is a prosthetic device that functions in place of lost photoreceptor cells. Although it does not restore normal vision, in clinical studies, the Argus II enabled people with RP to read large letters and navigate environments without the use of a cane or guide dog. In 2020, Second Sight ceased operations; the technology has been purchased by a different company which is pursuing a cortical implant, the Orion, rather than the retinal implant because some view the physical challenges of creating a stable retinal implant to be insurmountable.
CC LICENSED CONTENT, SHARED PREVIOUSLY
Lawrence Livermore National Laboratory, “Retinal implant seen as 2010 tech breakthrough”
URL: https://www.llnl.gov/news/retinal-implant-seen-2010-tech-breakthrough
License: CC BY-NC-SA 4.0
Wikipedia, Cortical implant
URL: https://en.wikipedia.org/wiki/Cortical_implant#cite_note-Fernandes-4
License: CC BY-SA 3.0
Wikipedia, Retinal implant
URL: https://en.m.wikipedia.org/wiki/Retinal_implant
License: CC BY-SA 3.0
Cheryl Olman PSY 3031 Detailed Outline
Provided by: University of Minnesota
Download for free at http://vision.psych.umn.edu/users/caolman/courses/PSY3031/
License of original source: CC Attribution 4.0

