Module 12: Intro to Mastitis Testing
Module 12.4: Special Biochemical Tests for Further Differentiation of Mastitis Pathogens
Further Differentiation of Mastitis Pathogens
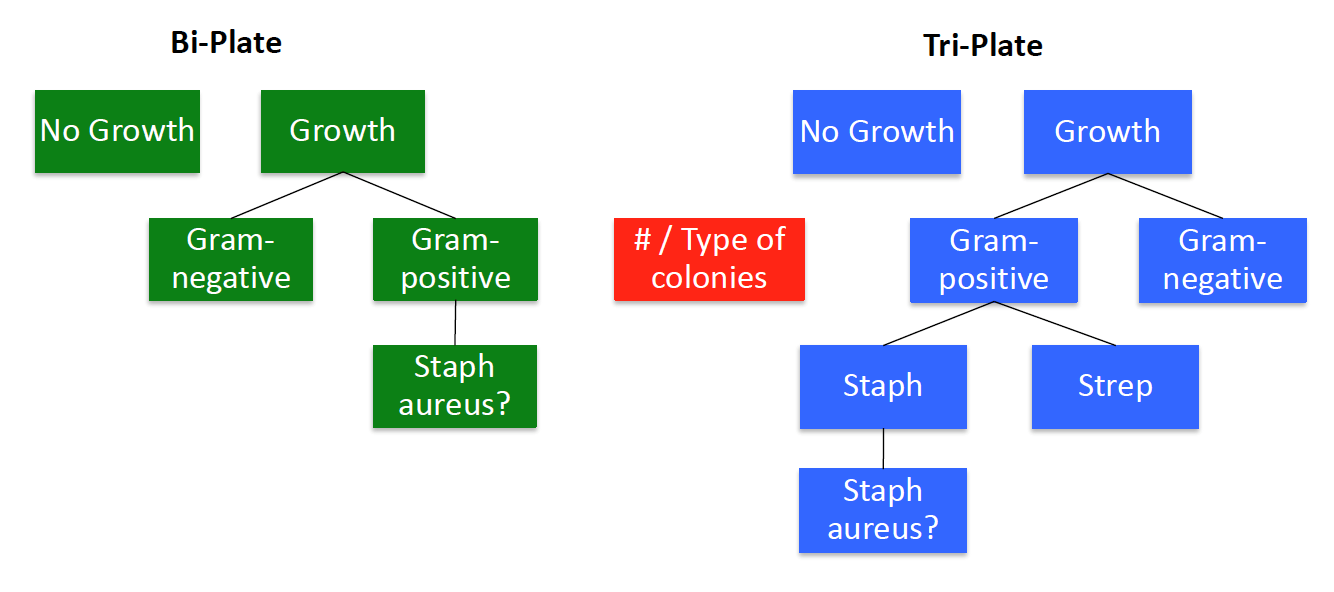
Once we have the mastitis pathogen narrowed down to Strep sp., Staph. sp., or a Gram-negative pathogen using the Bi-plate and Tri-plate culture plates, it is important to further determine their identity if possible.
The following sections will guide you through the steps for further characterization of mastitis pathogens.
Step 1: Growth or no growth
The first step to any bacterial culture is to determine if there is actual growth on your plates. It is especially important to not interpret milk globs or agar clumps from aggressive streaking as growth on your plates.
What if there is growth?
- Count the number of colonies and type of colonies (Gram +/-)
- If there are 3 or more different types of colonies seen, this is likely a contaminated sample.
Knowledge check
Step 2: Identification of pathogens
What if there is growth on all three plates with a single type of colony?
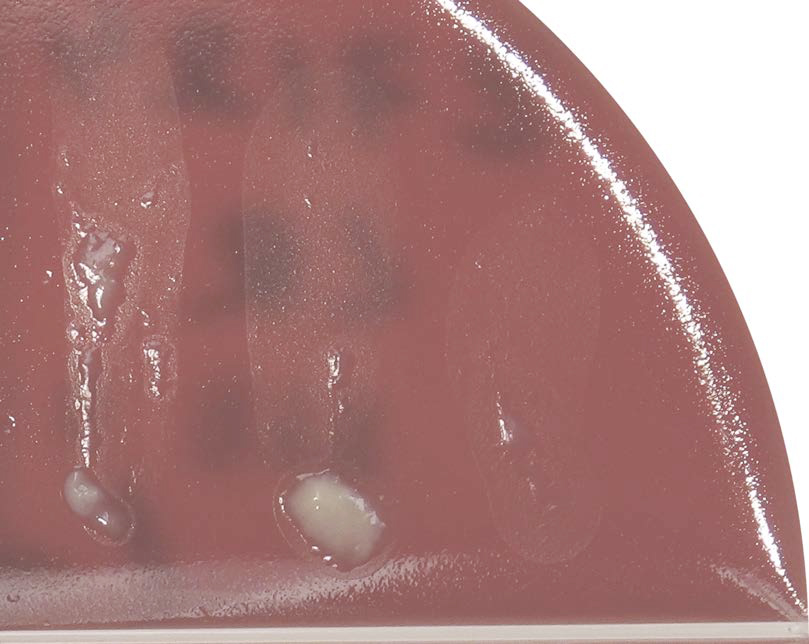
Prototheca
If growth on all sections look very similar and appear as small, dry whitish colonies we suspect Prototheca. Prototheca is an alga that is considered a contagious pathogen and will grow on many different types of media. Prototheca has devastating health implications for the cow so for this reason, we need to do additional tests to positively identify this pathogen.

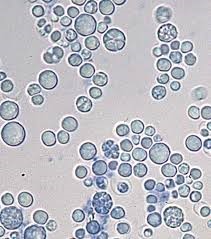
Prototheca has a very distinct microscopic morphology, thus if suspected we lift a few colonies from the plate and prepare a wet preparation. At 40x objective, these algae are round (about the same size as a WBC) with a Mercedes Benz or floral appearance to them

Knowledge check
What if we only find single colonies on one or more plates?
The first step is using our plates to attempt identification of the pathogen using our differentiating media.
Hemolysis patterns on the blood agar plate
Different mastitis pathogens have different hemolysis pattern of the blood agar plates[1]. The three types of hemolytic activity include:
Alpha (α):
Partial lysis of RBCs (cell membrane remains) resulting in a green or brown discoloration around colony from the conversion of hemoglobin to methemoglobin
Beta (β):
Lysis and complete digestion of RBCs surrounding the colony leaving a colorless area (I.E. Staphylococcus aureus)
Gamma (γ):
AKA non-hemolytic is the term referred to as the lack of hemolytic activity.

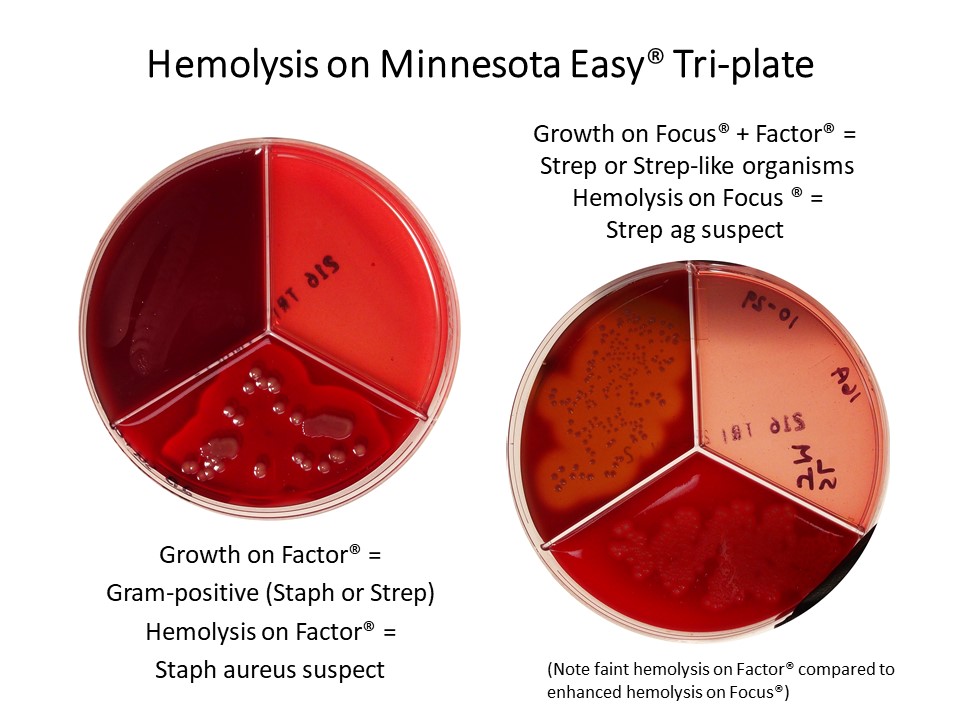
In the urine culture laboratory, we evaluated the different hemolysis patterns seen on our blood agar plates. Below are examples of the common hemolysis patterns that we observe with Staphylococcus versus Streptococcus spp. Other organisms can cause hemolysis (this is why we do additional biochemical tests).
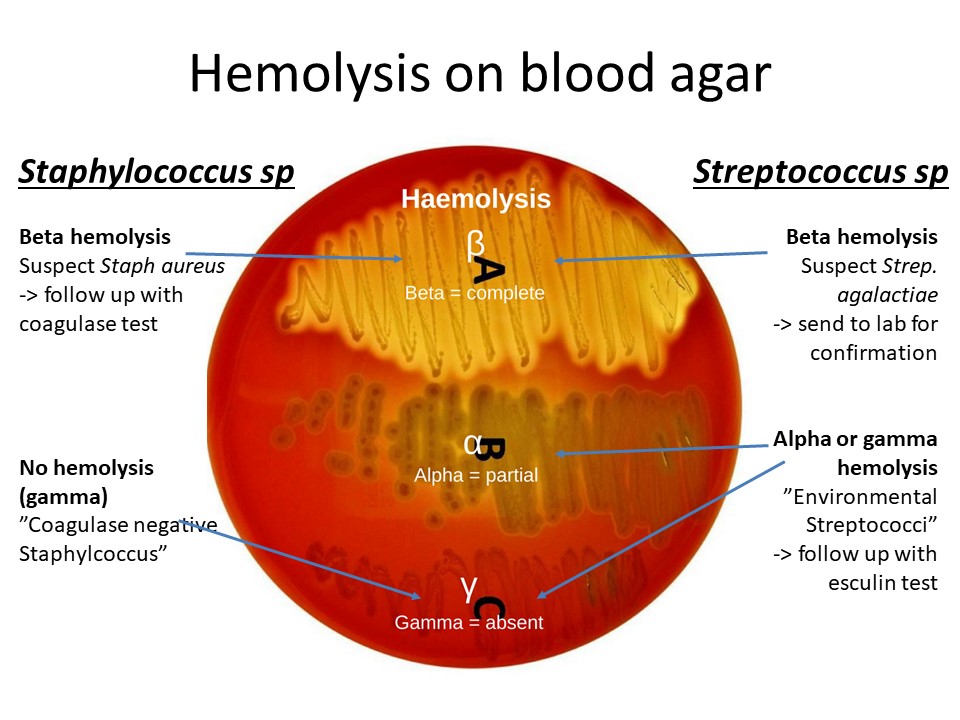
Minnesota Easy® Culture Media
The Factor® media (type of Blood Agar Plate) is enriched, differential media (gram-positive only) used to differentiate fastidious organisms and detect hemolytic activity. Factor® media is different from Blood agar in that it selectively enhances Beta hemolysis of Staphylococcus aureus, a significant mastitis pathogen. So colonies with pronounced Beta hemolysis on Factor® would be suspect Staph aureus, whereas on blood agar they could be Staph aureus or Strep agalactiae (or something else).
Focus® media is also an enriched, differential media, but selects for Streptococci and Strep-like organisms (Enterococcus, Lactococcus, Aerococcus) and enhances Beta hemolysis of Streptococcus agalactiae.
Knowledge check
Lactose Fermenters
As we discovered in the urine culture laboratories, the MacConkey media in addition to selecting Gram-negative bacteria it also indicator media as the lactose fermenting bacteria will form pink colonies.
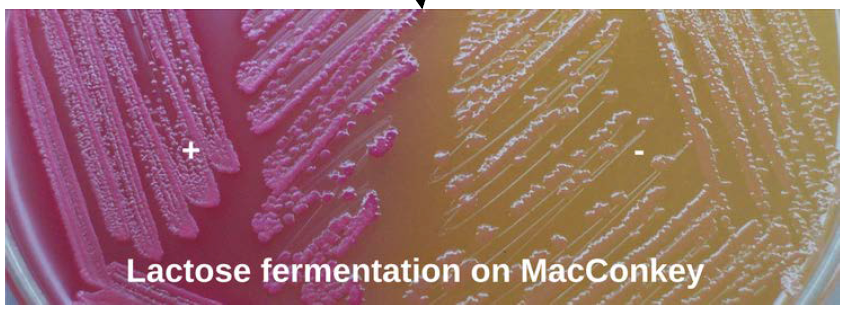
- If there are pink colonies, then these colonies are coliforms. The most common type of coliform is E. coli, but we would need to do additional testing to confirm that as other coliforms appear similar on MAC.
- If the colonies are white, tan, or grey, these are non-coliform Gram-negative bacteria
Knowledge check
Catalase testing
The catalase test is useful in the presumptive identification and differentiation of many bacteria, most notably Streptococcus spp. (catalase-negative) and Staphylococcus spp. (catalase-positive). Catalase is an enzyme that breaks down hydrogen peroxide into water and oxygen.
When catalase is present in the bacterium, when H2O2 is applied the colony will bubble. Bacteria that do not have catalase will not bubble. Here is a short video demonstrating this reaction.
While we are using this test to primarily differentiate between Staphylococcus and Streptococcus spp., other bacteria and yeast are also catalase positive. Using physical colony characteristics and differential plates is helpful to distinguish these other catalase-positive organisms.
Organism |
Catalase Reaction |
|---|---|
| Bacillus | + |
| Yeast | + |
| Prototheca | + |
| Trueperella pyogenes | – |
| Staph. sp. | + |
| Strep. sp. | – |
*Note that the Minnesota Easy® Tri-plate differentiates Staphs and Streps for you.
Knowledge check
Coagulase test
The coagulase tube test aids differentiation of S. aureus from other Staphylococcus spp. on the basis of their coagulase production. The test detects the presence of “free” coagulase, an extracellular protein enzyme that causes the formation of a clot when inoculated with plasma. Staphylococcus aureus is coagulase-positive. If a coagulase test yields a negative result, the Staph is placed into an umbrella grouping called “Coagulase Negative Staphylococcus” (CNS). Remember S. aureus is a contagious pathogen and CNS are environmental pathogens.

Video showing the “clotting” that occurs in the test.
Knowledge check
Esculin reaction
Culture media that contains esculin the (Focus®/MTKT portion of the Tri-plate in our lab) is used to differentiate Enterococci and group D Streptococci based on their ability to hydrolyze esculin. When an organism hydrolyzes the glycoside esculin to form esculetin and dextrose, the esculetin reacts with the ferric citrate in the media to produce a dark brown or black phenolic iron complex. A UV light may be used to more clearly visualize the reaction, although it can be seen without the UV light.

Esculin + |
Esculin – |
Esculin Variable |
|---|---|---|
| Enterococcus sp. | Strep agalactiae | Aerococcus sp. |
| Strep. uberis | Strep dysgalactiae | |
| Lactococcus sp. |
This is a useful test because the majority of esculin-positive Strep and Strep-like organisms (not Aerococcus) are typically more pathogenic than the non-ag/non-hemolytic esculin-negative Streptococcus dysgalactiae. Streptococcus uberis, Enterococcus and Lactococcus are more difficult to cure and more likely to cause chronic mastitis.
Knowledge check
Key Takeaways
- Most coliforms are lactose fermentors and detected on the MacKonkey agar
- Staphylococcus and Streptococcus can both have complete hemolysis (beta) on the BAP
- If you determine that the colonies are Staphylococcus or Streptococcus, the next step is a catalase test to differentiate
- If you determine Staphylococcus, the next step is a coagulase test to determine if it is an enviromental or contagious Staphylococcus
- If you determine Streptococcus, the next step is an esculin test and may aid in prognosis
- Prototheca grows on all types of differentiating and selective media. We use wet mounts for identification
- Focus plates are a type of blood agar plate. ↵
Umbrella term for bacteria that has originated from the GI tract. This is most commonly E. coli.

